Introducing BDI Briefs
I’m very excited to share the first episode of BDI Briefs! Together with Dr. Bill Polonsky and Dr. Susan Guzman from the Behavioral Diabetes Institute, our aim with BDI Briefs is to take a brief look at important issues about the emotional side of diabetes.
In this short discussion, Scott, Bill, and Susan talk about an interesting study from 2019 that found an association between primary care practitioner empathy and longevity in people with newly diagnosed type 2 diabetes.
There is a lot to unpack, and we only scratch the surface. But we hope the conversation is enjoyable and offers a few tangible takeaways for people living with diabetes and healthcare providers who care for them.
Enjoy! And please let us know what you think. We’d love to hear!
Detailed show notes and transcript
Scott K. Johnson: Hello and welcome to BDI Briefs. This is the first installment of what we hope to make a monthly series where we take a brief look at important issues about the emotional side of diabetes. Thanks so much for joining us today. I’m here with Dr. Bill Polonsky, President of the Behavioral Diabetes Institute, and Dr. Susan Guzman, Director of Clinical Education at the Behavioral Diabetes Institute. Both are world-renowned diabetes psychologists and two of my favorite people to talk with.
Scott K. Johnson: My name is Scott Johnson. I have lived with diabetes for over 40 years and have been active in the diabetes social media space for a couple of decades, and with introductions out of the way, Bill, what have you got for us today?
Bill Polonsky: I’m really glad we’re starting to do this, Scott. I’m really glad you’re here, and I’m really glad Susan’s here, and I hope as we do this every month, we’re going to be talking sometimes about our own research, we have some new publications, as well as really cool things we read about in the recent literature that we think are really relevant to what we do here at BDI.
Bill Polonsky: And we thought we’d start this month with one of my favorite studies. It was actually published a couple of years ago, in 2019, but it’s so important I just want to make sure everyone knows about it. First author is a woman named Dambha-Miller.
Bill Polonsky: And this was a wonderful study. It’s from the United Kingdom. And what they did in this study they had more than 600 people with type two diabetes, all of whom had been diagnosed within the past year or so. And they asked these 600 people to fill out a very brief 10-item questionnaire.
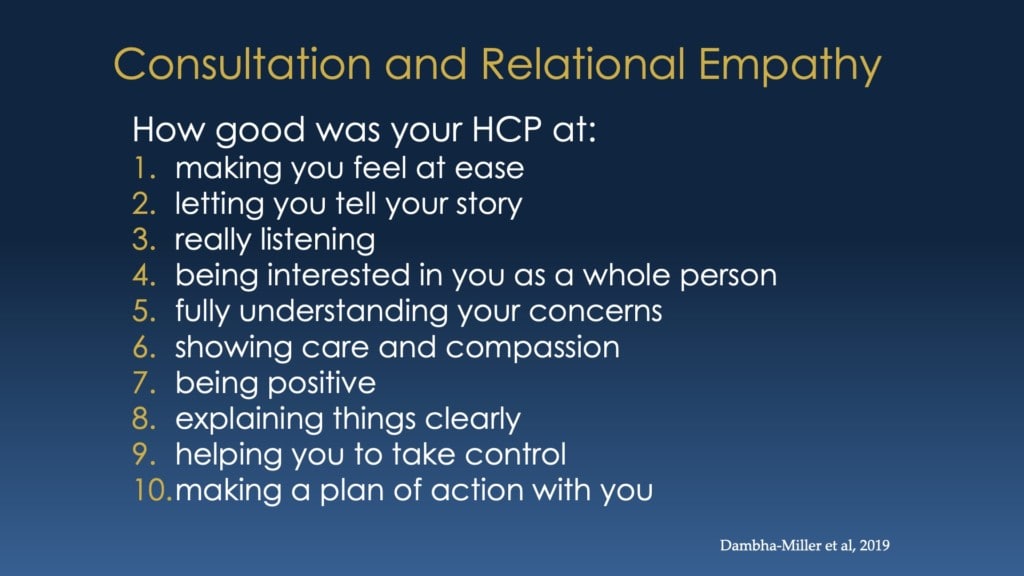
The questionnaire was really having to do with; So what do you think of your healthcare provider? What do you think of how your healthcare provider treats you? And in particular, it was looking at empathy, trust, sense of collaboration. There were questions like, how good was your healthcare provider at making you feel at ease, letting you tell your story. Really listening, being interested in you as a whole person, the individual would rate each of those, these 10 items and you’d have a total score.
Bill Polonsky: But what’s really awesome about this study is they then followed these people for ten years, and the question this study asked was gee, I wonder if, how people filled out this questionnaire– in other words, their statements of the sense of connection and trust and collaboration with their healthcare provider– was related to how well they’re doing ten years later. And they looked at very hard clinical outcomes. And I want to talk about one of those clinical outcomes in particular, and I think we can all agree it’s a pretty good one, and that’s death.
Bill Polonsky: And what they found was that people who scored high on this questionnaire who said, you know what? I really do trust my healthcare provider. I really do feel like my healthcare provider is listening to me. Their likelihood of being still alive ten years later was almost doubled. In fact, I’m going to read the slide.
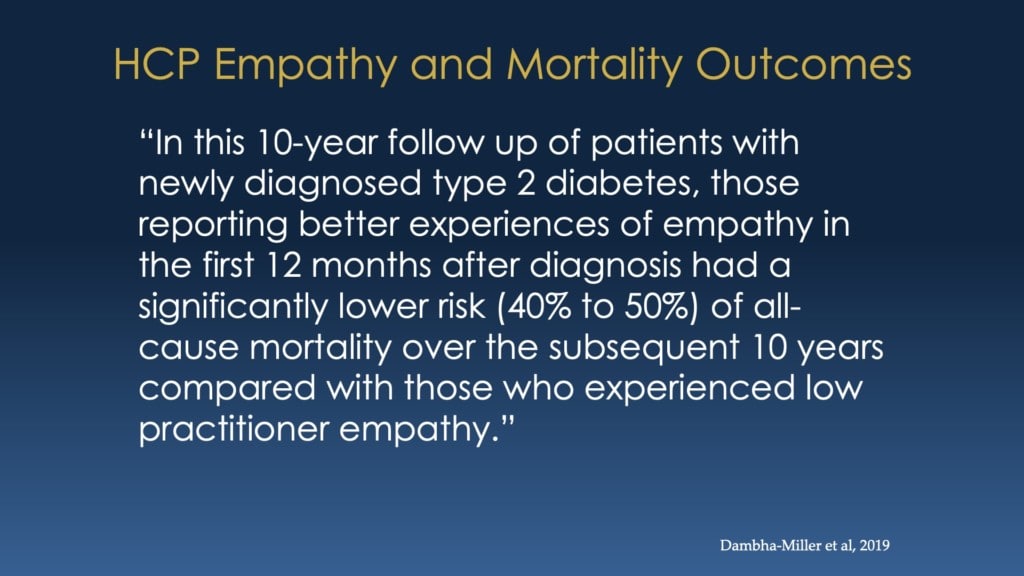
Bill Polonsky: It’s a bit jargony, but it’s important because it really says this so clearly. Here’s what it is. In this ten-year follow-up of patients with newly diagnosed type two, those reporting better experiences of empathy in the first 12 months after diagnosis had a significantly lower risk (40 to 50%) of all-cause mortality, over the subsequent ten years compared with those who experienced low practitioner empathy.
Bill Polonsky: So that’s wordy, but you can see in the parentheses this 40% to 50%. This is mind-boggling. There have never been studies like this before. Think about what that means, whether you’re a person with diabetes or whether you’re a healthcare provider. I mean, this really suggests if you have a relationship with your healthcare provider or your relationship with your patients, you really have this sense of connection and trust and empathy that, that your doctor, your nurse, your PA is really listening to you. It might double the odds you’re still alive ten years from now. That’s amazing.
Bill Polonsky: Now it’s only a single study, and as researchers, we have to say we, we’d like to see this rep replications. We’d like to see further studies, but still, this is incredible. So that’s what I wanted to mention, and I’d love to hear, Susan, I want you to chime in. Scott, I want you to chime in. Let’s talk about this kind of amazing study.
Susan Guzman: Yeah. I’d like to think about two things. One is, what is that really about? Like when, if you feel like you have a caring, listening, empathetic, engaged healthcare professional, how does that double your risk of survival when you have diabetes? What is that really about?
Susan Guzman: And the second thing is how do we do more of it? And Scott, I would also like to think about like from a person with diabetes perspective, you obviously can’t fix your healthcare professional, but, what can you do besides just find another doctor?
Susan Guzman: And maybe that’s all, maybe that’s all you can do if you find that you’re not connecting. But I’m really interested in maybe discussing what you think that’s really about? When you have an empathetic healthcare professional? How does that matter so much? And now, we have some thoughts and other studies that we can pull from to make some good guesses.
Scott K. Johnson: Yeah. I think the first thing that comes to mind for me is that you feel as a person living with diabetes, that you’ve got someone on your side. I think of a common experience in type two diabetes is a lot of guilt and shame and stigma and blame, sometimes unnecessary. Sometimes founded. But, there are a lot of emotional aspects there.
But if you feel like you’ve got someone on your side, someone on your team that, that can really help you through that, I think that’s a big deal and a huge motivator to keep trying and keep going forward. But you’re right. And that there are times when I think the best solution is to find a different provider. But I think that’s pretty extreme too.
Bill Polonsky: And, you bring up something important, Scott, which is, hey, we’re talking about a group of people with relatively newly diagnosed type two diabetes. Will this matter for other groups? And thinking of you, will it matter for people with type one diabetes? We’d sure like to think so. And it would make sense, but we don’t know.
Susan Guzman: What makes me think that it will, Bill, is that it was related to all-cause mortality. So it wasn’t just specific diabetes-related outcomes, like cardiometabolic stuff, yes, but it was also other things. It leads me to think of the other studies Bill that you’ve talked so often about in some of our training programs is that how important trust is to whether you engage in following the recommendations from your healthcare professional. Especially around medication taking.
Susan Guzman: So if you trust your doctor, you feel like they’re listening and they have your best interests at heart, then maybe that medication they’re recommending to you really isn’t a bad idea, that you’re willing to trade side effects or an expense or the willingness to be on medication because you know that doctor is really, he or she is on your team. They really get where you’re coming from, and they are working for you and with you.
Scott K. Johnson: And I think that most of the time that, that can be said for all doctors, but it’s the feeling, the perception that the patient has about whether that’s happening or not that seems important here, right? I think that’s an important call out. I’ve never met a doctor who didn’t have their patient’s best interest in mind, but whether that feeling is conveyed to the person across the chair or the exam table makes a big difference.
Scott K. Johnson: So, with that in mind, what does it look like for a healthcare provider to maybe be on the receiving side of good scores around empathy?
Bill Polonsky: What does it look like? I think it’s an important question because we know that many healthcare providers, if they’re listening now even are thinking, “oh, you gotta be kidding. I don’t have time. I don’t have time to hang out and be that pleasant.” And even though they’d prefer to be right, but again, there’s just such enormous pressure with stuff to fill out and the waiting room full of folks. And I think you’re alluding to this, we know that to create that atmosphere, It doesn’t have to take time.
Bill Polonsky: It is a way in which you spend time with folks. It has to do with how the furniture might be arranged in the room where you see someone. Are you sitting across from a desk from them, for example? Are you sitting next to them in any point in time? Do you actually look at the person you’re meeting with, or are you just staring at your screen and filling out stuff on your computer screen?
Bill Polonsky: Are there a few moments where in any way you, as an overwhelmed, busy healthcare professional, can look at the person in front of you, even if it’s just a few seconds, and say, this is a person, not just a series of numbers. And I don’t mean to say it’s easy, but it doesn’t have to take a lot of time. Susan and I spend a lot of time training healthcare providers about how on earth you could possibly come alongside your patients without it having to be onerous, without it having to be burdensome. So yeah, it’s an important issue. We think that’s why we’re talking about it now.
Susan Guzman: Yeah. I talked to a healthcare professional yesterday, a really great endo who trains fellows in her program and she was saying how she thought that addressing the emotional component was so critical and whether people are able to, to not only. Positive medical outcomes, but also like how important recognizing quality of life and emotional well-being is in overall diabetes management.
Susan Guzman: And I said, you’re kind of a unicorn for saying that out loud and recognizing that’s key and. And she laughed and she said I’m sorry to hear that. And she goes, I do have the reputation of being one of the more emotionally focused, touchy-feely people. But she said, she has decided that it’s important as a leader in her team anyway, that to create a culture, that’s what’s expected, that we treat people with dignity.
Susan Guzman: She even used the word love – come from a place of love, and always remember always that there’s a person sitting in front of you, and she says, then the rest comes more naturally. You tend to listen more when you’re looking at a person and not a diagnosis or numbers, not lab results, but to recognize, she said also, and I thought this was really important as well, that diabetes is tough.
Susan Guzman: So, if you recognize diabetes is tough, having, if the person’s having challenges that’s not abnormal, that’s expected.
Scott K. Johnson: You know what, I think that’s a big point. Yeah. That it’s tough and that it’s normal to have challenges and a number of failures mixed in with whatever successes you’re finding.
Bill Polonsky: It’s funny, and if you look at the items where the individual would score their relationship with their healthcare provider, one of them is that you feel that your healthcare provider really takes the time to listen to your story, not fix everything, just listen to your story.
Bill Polonsky: And one thing I didn’t mention about that really remarkable study is when they really looked even more in detail at the scores, there were, at how the individual would score their relationship with their healthcare provider and how much that meant. What really stood out was really low scores that mattered, meaning the people who were most likely to have higher rates of all-cause mortality were those who scored their healthcare providers very low.
Bill Polonsky: And that’s important because it means you don’t even have to be as a healthcare provider, terrific at this. You just have to not be terrible. And just little things like the ways we’re talking to let your patient know that you’re on their side or making that effort can make a, apparently, if you believe this crazy study, can make potentially an enormous difference.
Scott K. Johnson: I think that brings up a big point too in that, if I feel like my doctor is not even on my side, then the negative, the negative conversations I’m having in my brain with myself, they just run rampant, and it’s this kind of downward spiral that’s pretty destructive, I think. It’s important to feel that someone’s on your side and cares about you.
Scott K. Johnson: It doesn’t have to be about time necessarily, but one example that comes to mind is if we made a medication adjustment in a previous visit, the healthcare professional can typically see some data results in lab studies or what have you, blood sugar numbers, whatever. But even just simply asking, how’s that going? How is that adjustment working for you? It is a big deal to find out if there’s anything that I’m struggling with.
Susan Guzman: Yeah, that’s really good. Yeah. We interviewed one of our favorite endocrinology practitioners and he said when he’s reviewing numbers before he gives any feedback, regardless of what he sees on the paper, he always says, I see how hard you’re working. And that was like magic for people who heard it.
Susan Guzman: Yeah. That really goes a long way because it is a lot of work. Whatever you’re doing on your diabetes it’s a lot of work. And diabetes is one of those things where, the outcome doesn’t always reflect the level of work put into it, especially if you’re not on the right mixture of medications or there are other things going on. So I think that’s a really huge statement.
Bill Polonsky: Scott, let me put you on the spot as an N of one on this call. So even though you have type one, not type two diabetes, I’m pretty certain you’ve probably. Really positive experiences with healthcare providers and odds are pretty good you’ve had less than positive experiences with healthcare providers and anything you can tell us about your own experiences where either way it made a big difference or affected you?
Scott K. Johnson: I remember having an endocrinologist who was very data-driven, and I am more of a touchy-feely guy, and so I, I needed a clinician who would check in with me a little bit more about my emotions and the emotional side of living with diabetes and not just going through numbers and data.
Scott K. Johnson: And I, I feel like I tolerated that relationship for a while before I decided I just had to, I just had to change to a different endocrinologist. And that was a really big decision for me. It’s not easy to change clinicians. And especially if you’re in a situation where there aren’t many to choose from.
Scott K. Johnson: I was really blessed in that I was at a larger clinic. But you know, making that change to someone that had a little more touchy-feely bedside manner, if you will, was a big deal. And that really helped out a lot. I think I also learned along the way that there are things I can do from the patient side to help facilitate that relationship.
Scott K. Johnson: So one of the things that, that I try to do is come in with a short list of questions or concerns so that we can address those together. And at the end of the visit, I feel like I’ve accomplished everything that I need to accomplish out of that. While also recognizing that there are things that the clinicians need to accomplish during their visit too.
Scott K. Johnson: They have almost a rubric, if you will of things that they need to do during that visit. And so it’s really a balance back and forth between the two of us.
Bill Polonsky: I like how just by bringing in a list of comments, questions, or things you want to bring up can potentially instigate more of what you need. That your questions or your comments are going to be more than, “let’s talk about how we’re going to fix these numbers.” It’s going to be about me as a person. And again, I think some of your examples that you mentioned before are so perfect, right? So it’s lovely that you would have an endocrinologist who would want to focus on your numbers, but then you do just a little bit more than that, like you said, Hey, you know, we made that insulin change, what do you think of that? What’s it been like for you? What’s working for you? What’s not? Just something that simple can shift everything.
Scott K. Johnson: Yeah, absolutely. I think too that along with that comes an opportunity for the clinician to maybe better educate me about things that may be expected side effects, or if I’m struggling with something. They can say, yeah, we’ve seen that before. Still, if you, you know, we can make this adjustment to a different, a different flavor of that medication to try and help that or, typically if you just stick with it for another couple weeks, the side effects will subside.
Scott K. Johnson: Things like that. It’s really opened up a lot of education opportunities for me, and I think that pays big dividends both from the patient side and the clinician side.
Bill Polonsky: Yeah. Susan, what do you think? Other comments, thoughts?
Susan Guzman: The only other comment I have would be I guess the opportunity of last resort and that is if you really are trapped within someone who is in that awful category as a person with diabetes, and that’s your provider, and you don’t have options.
Susan Guzman: I think recently, especially, we’ve heard some stories from people with diabetes or other healthcare professionals that have, who’ve had people that they work with who had a really terrible experience, and they were brave enough to speak up. And it’s really hard because, in navigating my own healthcare, I know that times when I’ve tried to do that, sometimes it went well, and many times it didn’t.
Susan Guzman: But, I think it’s a nice opportunity sometimes for you if you work out a way to say, like when you said that, you know, that I’m doing a bad job, or whatever it was that they said, that, that wasn’t helpful.
Susan Guzman: I feel like sometimes when the best lessons for healthcare professionals come from when patients are brave enough to give them feedback about that respectfully, that wasn’t helpful.
Scott K. Johnson: Yeah. See, that’s a really interesting point. The other thing that comes to mind too for me is that growing up with type one diabetes, my endocrinologist was typically the quarterback of my healthcare team.
Scott K. Johnson: Whereas, you know, someone with type two diabetes, it may be more of a family practice doctor or a general practice clinician. But that the relationship with whoever’s really driving your healthcare team is really critical and important and. Be brave enough to think about what you need from that relationship above and beyond prescription refills or lab test reviews. That’s a big step, but it can really go a long way.
Susan Guzman: Yeah. Not easy to do, I do recognize that though.
Bill Polonsky: it might be a, what you just said, Scott, might be a good way for us to wrap things up. It’s so fascinating when I think about it. We’re so used to saying, the time you spend with your healthcare provider over the course of a year is really little, and so much, the vast majority of what diabetes is about is what you’re doing on your own every day.
Bill Polonsky: And yet, here we are talking about this study that says, you know what? That tiny amount of time you spend with your healthcare provider might be so important. It might have a dramatic impact on your longevity. On top of everything else, I mean, that’s impressive, and it really highlights why I think it’s important for us to be talking about this and sharing this with everybody.
Scott K. Johnson: Thank you for helping shine a little bit more light on this. We’re planning to do this on a regular basis. So folks, please let us know what you think about it. If there are things we can do differently if there is maybe some research you’d like us to take a look at.
Scott K. Johnson: I know that Bill and Susan have a long list on the docket already, but we’re definitely open to feedback. With that, thank you for spending a little bit of time with us today, and we will see you soon next time. Thanks, everyone.