"AH-HA!" moments in diabetes education
Welcome to episode 2 of BDI Briefs! Our aim with BDI Briefs is to take a brief look at important issues about the emotional side of diabetes.
In this short discussion, Scott, Bill, and Susan discuss innovative ways to transform diabetes education by creating “AH-HA!” moments in group education sessions. I also encourage you to look at more research from the Behavioral Diabetes Institute.
Enjoy! And please let us know what you think and what you’d like to hear more about from BDI.
And remember to subscribe to BDI’s YouTube channel!
Detailed show notes and transcript
Scott K. Johnson: Welcome to BDI briefs. This is another of our monthly series where we’re taking a brief look at important issues about the emotional side of diabetes. Thanks for joining us today. I’m here with Dr. Bill Polonski, president of the Behavioral Diabetes Institute, and Dr. Susan Guzman, director of Clinical Education at the Behavioral Diabetes Institute.
Scott K. Johnson: Both are renowned diabetes psychologists and, again, two of my favorite people to talk with. My name is Scott Johnson. I’ve lived with diabetes for over 40 years and have been active in the diabetes social media space for a long time. With introductions out of the way. Bill, what are we talking about today?
Dr. Bill Polonsky: Thanks, Scott. I’m just so glad to be here with both of you. So we’re going to talk about, actually, one of my very favorite subjects, which is about, well, some new ideas about how we can transform diabetes education. And we want to talk about, or at least we’re going to lead to talking about, a particular publication that came out just a few months ago.
Dr. Bill Polonsky: And not to toot our own horns, but well, we wrote this and it’s our project. So we’re very excited to talk about something that I don’t think many people have even heard about yet. And of course, and the reason we’re talking about this is that we really see that there’s a huge need to transform diabetes education, and we’re going to be thinking about it for people with type two diabetes, but I think it’s going to make sense for people with type one as well. And the reason we decided the transformation was needed is that in our travels around the country and with people we talk to, what we’ve seen is that diabetes education programs, group programs are often, well, kind of boring.
Dr. Bill Polonsky: I mean, not all the time, but often they really are. And we know that people don’t stick with them. They drop out, and they may not get out of them what they need, even though we have pretty good evidence that diabetes education programs, if people do stick with them, really can help people to feel better about diabetes, manage diabetes better, and get more engaged.
Dr. Bill Polonsky: But clearly, there is enormous room for us to do a better job. So we want to think about it both from the perspective of healthcare providers, especially diabetes educators, and we want to think about it from the perspective of people with diabetes. So let me tell you a little about what we set up, and then we’ll get Susan to talk about her incredibly important role in this.
Dr. Bill Polonsky: So what we set out to do is we began to think about how could you possibly make diabetes education in a group format more interesting and engaging to more meaningful to people. We realized we had to integrate continuous glucose monitoring in some fashion. Let’s face it, hearing a lecture from an educator about why you should eat better, or here’s some plastic food to look at that you should try, or exercise is kind of valuable.
Dr. Bill Polonsky: The lecture thing doesn’t work as well as personal experience. So when people can have their own glucose monitor, especially a continuous glucose monitor, and go home and try their own experiments in a structured way, which is what we do in this program to find out gee, I wonder how breakfast affects me, or wonder what exercise does.
Dr. Bill Polonsky: And when you actually see it for yourself, that’s when it moves the needle. And that’s when we see for all the people we work with, and actually, even when I’ve used these systems, that’s when it becomes real and really makes a difference. What we set out to show is that this could really work. So we did a small single-arm pilot study.
Dr. Bill Polonsky: It was pretty small. It was only about 35, 36 people in small groups, and we figured to do this right, we probably should make sure we engage with group facilitators who know what they’re doing. So we found two people. One was one of the most prominent and well-known diabetes educators in the world. Her name is Marty Funnell, who’s just wonderful.
Dr. Bill Polonsky: Then we looked everywhere for a behavioral expert who could join and work with Marty. And we found this woman named Dr. Susan Guzman, who happens to work with us. So Marty and Susan worked together in these small groups to make a big difference. So what did we do? What happened to folks?
Dr. Bill Polonsky: Well, we’ll tell you a little later about the study results, but I’m going to turn it over to Susan to tell us about what she and Marty did, and what they saw.
Dr. Susan Guzman: Well, everyone was wearing a continuous glucose monitor, and we started introducing them to basic concepts to help them think through what they were about to see.
Dr. Susan Guzman: So we introduced them to, at first, the 5 Ms, which are, let’s see, Scott, if you can, if you would, if any of these will surprise you, I won’t put you on the spot because two of them always stump people, but Medications, Movement, Meals, Mood, and the last one is always like, what? And it’s Minutes. And minutes has to do with the timing of all of that stuff.
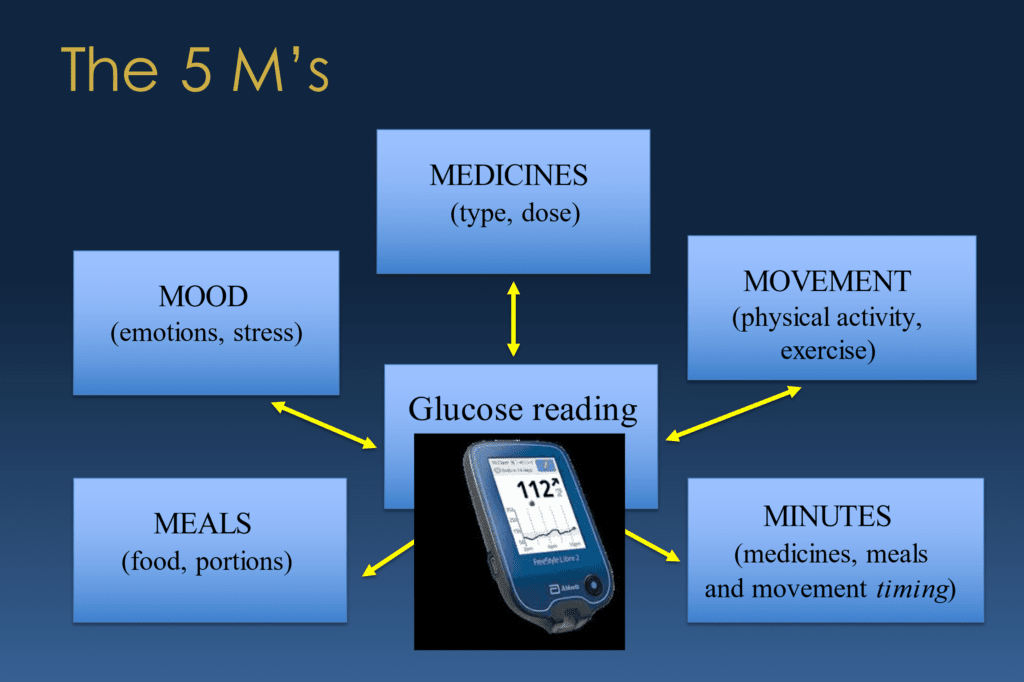
Dr. Susan Guzman: And, we always encourage people to think of when the mood one is kind of, we forced an “M” there, but it’s not just stressors that affect, you know, your, psychological stressors, but also physiological stressors like getting sick or having surgery or, you know, things of that nature. Even sleep we put under Mood because that’s a physiological stressor when people get inadequate sleep.
Dr. Susan Guzman: So, but to help, so introducing people to, like, these are the, when you are looking at these numbers and to be thinking about which of the five Ms or what combination of the Ms might be having an impact. And then we ask people to do experiments and have it about something that actually interests you.
Dr. Susan Guzman: You, you’re wanting to find the answer to, like, how do my breakfasts affect me? Or, you know, that exercise that I occasionally do, does that actually even matter to my blood glucose numbers? And then sometimes people would do experiments sort of on accident cause they sometimes would do their routine medications and sometimes they’d forget and go, guess what?
Dr. Susan Guzman: I forgot my medication for two days. And I noticed that really started showing up in my numbers. And so sometimes people would have what we were calling “AH-HA!” experiences on accident. Like I forgot my medication. And boy, did it show. We weren’t encouraging people to play around with whether or not they take their medication.
Dr. Susan Guzman: But, you know, life happens to people. And so then we started explaining, how do you… I think one of the most valuable things that CGM allows people to do is to help keep their numbers in perspective. So where one meal you might go, “oh, I really blew it”. And you start to feel hard on yourself, but then when you start standing back and say, “how did that fit into my week?”, “When I look at my time and range for the week, did that even really matter?”
Dr. Susan Guzman: And so starting to look at, you know, what, how do you interpret the ambulatory glucose report, the AGP report. So when you look at it like, what does it mean? How do I interpret my numbers? How do I look for patterns? Where do I focus my action? Just started to use it as a tool to help guide choices.
Dr. Susan Guzman: And at the end of the day, what, what we were most hoping people were going to start getting out of it is, how do they look at their numbers in a way that helps them make choices? And we think about choices both as informed choices. So I know that when I eat rice with my dinner, for example, my blood glucose is gonna go up a certain amount.
Dr. Susan Guzman: But also what Marty Funnell referred to as a wise choice, which is how does, how do my choices not just impact my diabetes? But my overall life? Like sometimes, you know, like, you know that a birthday cake is going to raise your numbers, so you can make an informed choice whether to have that or not.
Dr. Susan Guzman: But a wise choice also respects the fact that you’re more than just your diabetes and maybe the birthday cake is a good choice for you at that moment. So getting away from thinking about, you know, numbers again, as good or bad, or even choices is good or bad. They’re informed and wise, and we want people to consider, you know, really leaning into making choices without judgment.
Dr. Susan Guzman: And we encourage people to share their experiences without judgment. And I think another key ingredient to this was that there are no stupid questions. And so, people felt, I feel like really more empowered to share what they’re really doing and not doing because we’re really working from a no-judgment approach.
Dr. Susan Guzman: I mean, we have a slide just dedicated to that. No, this is a no-judgment zone.
Dr. Bill Polonsky: Hey, Susan, let me, let me add something that I think is so important. I don’t want you to skip over in terms of what you did that was so wonderful. The other thing is that there were no lecturers involved in this. That almost everything you and Marty were doing was really based on what people brought in. Their questions and their concerns, and ensuring that what they discovered and were interested in was being answered.
Dr. Bill Polonsky: And that chaos, if you will, made it important for folks because we’re talking about their stuff, not some just highfalutin lecture that somebody wants to give. And I think that’s embedded in what you’re saying, but I just want to make sure everyone understands that.
Dr. Susan Guzman: Yeah, and I think that related to that, so you know, when questions around diabetes aren’t just around blood glucose numbers, right?
Dr. Susan Guzman: And so that was the other, you know, really important point. Like sometimes people would say, you know, most people don’t know I have diabetes and this thing (glucose monitor) beeped, and then I was suddenly put in this position about what do I share about it? And I’ve never done that before. And so it would start to bring in all, you know, other aspects of living with diabetes beyond the glucose numbers.
Dr. Susan Guzman: And yeah, I think that’s also, yeah, a really important point. And when you have an educator like Marty who has done education classes for decades, you know. She knew the important points to raise if they didn’t come up in conversation; like saying, we haven’t talked about blood pressure.
Dr. Susan Guzman: Has anybody wondered or have questions about what role blood pressure plays and why they seem to ask you about it when you have diabetes? So, I mean, you can ask good questions and get them to, you know, engage with topics. So, I mean, there is a way to bring in sort of, you know, a more classic agenda without scripted slides.
Dr. Bill Polonsky: Can I, can I add the other thing that you guys had to do that I think made this some more challenging, which even is going to be more striking when we talk about what we found, was that this was all online. This wasn’t a bunch of people sitting in a room. You did this all online.
Dr. Bill Polonsky: Many people were sitting in their own homes, and you just had this video connection partly because we started this in the middle of the pandemic. That was a challenge you managed to figure out and keep the people engaged even though they were, well, kind of like what we’re doing right now. I think that was extraordinary.
Dr. Susan Guzman: Well, the cool thing about that. The cool thing about that zoom thing is that it actually allowed me to pull up their reports, their glucose patterns. And we could look at them and pick them apart as a group. Like, Hey, what do you think? What did you see? And how might that be different than Joe’s?
Dr. Susan Guzman: You know? And that was kind of, that was a cool thing that, that we were able to do because it was virtual. I mean, you could do that in an in-person setting too. It’s just a little trickier maybe.
Scott K. Johnson: I think the thing that, that jumps out to me about that, so just kind of zoom, there’s so much I want to talk about with this, but I want to zoom in on the, on the remote piece. You had a pretty good percentage of participants who made it to every session. I think to myself about how many cool things I sign up for that I can join remotely, but when it comes time to actually do the thing, I find an excuse around the house not to join, or I’m too tired, or whatever.
Scott K. Johnson: So I think that speaks highly about the amount of value they received from the program.
Dr. Bill Polonsky: Here here, yeah. So we have a little more time. I hope so. I want to take a few minutes and talk about what happened. And again, this was a small pilot, so we weren’t expecting much. We were truly collecting information in this single-arm study to hopefully get enough informa…, learn enough so we could figure out how we could do a larger formal, randomized controlled trial.
Dr. Bill Polonsky: So we have some interesting results, but before we talk about the actual numerical results, I think what’s more important, and I’d love to hear what Susan has to say about what people told you, told us about how this made a difference for them and what were those, “AH-HA!” moments. By the way, I should mention this whole thing was called the “AH-HA!” project because that was our goal.
Dr. Bill Polonsky: What do you think, Susan? What stood out to you about people’s stories? What’d you hear?
Dr. Susan Guzman: I think one of the things that we were curious about was, do people who are not on insulin and have type two diabetes find value in cgm. And I have to tell you. There were grief reactions when it was time to end the study and they had to stop using cgm.
Dr. Susan Guzman: One man, I thought, put it so well, he said, “it’s like I’ve been trying to navigate in a dark room, and I got to see what was, what it was like with the light on.” You know, when you have, when you’re able to make choices when you can see when you’re navigating it, it makes it a whole lot easier.
Dr. Susan Guzman: And he says, “I feel like I understand my diabetes so much differently than when I was just doing finger sticks here and there, what was happening to me at night, or times when I wouldn’t normally check, and just to make sense of numbers.” And so that was a big one. Is this how much people valued CGM when they’re not on insulin, and those are the people they get it paid for in general. Right?
Dr. Susan Guzman: So, you know, it’s, these are, these are devices that I think are game changers across the board and, and so far, that’s not necessarily what people are going to be able to utilize, you know, as of yet. Another thing I’ve heard a lot of Bill that, that I’m, I was kind of bummed and it didn’t show, is people were changing their relationships with their medication.
Dr. Susan Guzman: They said, you know, I take this medicine. I don’t really know what it does. And you know, they had some vague idea that it helps with blood glucose without really knowing why. And sometimes they’d say, yeah, it’s kind of easy to skip because I don’t really feel any different. And all of a sudden, they started seeing the value of it and discussing about it.
Dr. Susan Guzman: Like, gee, like some of the people who weren’t taking medication, were, they were on their exercise bikes, like an hour a day, and they were not having any movement in their numbers. And then, start a medication and all of a sudden their time in target is, you know, 80% or something like that.
Dr. Susan Guzman: And so it’s like, you can’t, you can’t outrun a pancreas that needs some help. So I felt like there was a big shift in that and just sort of, again, being able to make choices about food, exercise, and just understanding diabetes from a way that, you know, we’re really understanding what goes into it.
Scott K. Johnson: I love the comparison of navigating around a dark room versus, oh, here, the light’s on now. Like, how can you possibly make an informed or wise decision when, when you can’t see anything, right? So you flip the lights on and, okay. All of a sudden I have a lot more information to work with.
Scott K. Johnson: And I think the other thing that really stands out to me about all of this is the five Ms, which is, is something I had not heard of until this, and the fact that, you know, sure. Medicines, Meals, Movement, that all makes perfect sense. But I think it really actually takes a lot of pressure off by adding Mood and the Minutes and timing. Right?
Scott K. Johnson: So learning that here are a bunch of things you may not necessarily be able to control, whether you’re sick or whatever, how those affect what you’re seeing with your, with your diabetes. I think it’s brilliant.
Dr. Bill Polonsky: So I should mention that, you know, our goal, and I think we did this fairly well, is the people who were in this program all had type two and they were relatively new to type two diabetes. The whole idea was to see if we could catch people early on in the course of this disease, and who had elevated blood sugars to begin with. So, that’s the population I think in particular we hope, wow, we could really help make such a huge difference of people helping them, you know, get off on the right foot, helping them to really be engaged.
Dr. Bill Polonsky: And again, as I mentioned, to our surprise, even though we didn’t expect so. We did see a quite significant improvement in glucose outcomes over the course of three months. We saw, for example, time in range improve, and by the way, we’re looking at this using blinded CGM for several weeks before the program and blinded CGM afterward at this three-month, outcome. Time in range improved a lot, time above range, again, above 180 milligrams per deciliter was almost cut in half. And also, when we looked at patient-reported outcomes, we looked at quality of life. Again, we saw well-being significantly improved. We saw diabetes distress drop, although it didn’t quite make our p-value of significance, we saw, as Susan said, we saw people making changes.
Dr. Bill Polonsky: I think our measures of asking people about behavior weren’t so good, but we saw definitely people were making changes in how they eat and how active they are. And to some degree, actually in their medication use. It’s enough to help us understand how we can ask these questions better and do a better job once we get funding for doing this larger randomized control trial to really show that this really new approach is significantly better than our old way of doing diabetes education, which involves, again, not just using CGM to bring diabetes education alive, but when you do it the way that Susan and Marty did–when it’s based on answering people’s questions, it’s not just giving lectures–and you put all that together. Even if you do it online, we’ve seen remarkable results, and I hope we’ll see better in the future as well. I don’t know.
Dr. Bill Polonsky: Susan, what do you, any other thoughts about this or turns out what you did and what you saw?
Dr. Susan Guzman: No not really. I think you captured it.
Scott K. Johnson: You mentioned something else I think is really important to call out and, and this with this, this method of, of education was very personalized. Helping people arrive at their own “AH-HA!” moments. Right?
Scott K. Johnson: This is a much different experience than someone telling you, Hey, this and that should equal this. Right? It’s, it’s a much different experience than lectures and, I think that there’s a lot to that. Finding ways to navigate education in that manner in groups is, is important and deserves a lot more attention because it’s, it’s clear to me that it works well.
Dr. Bill Polonsky: And I also hope it opens up, it will open up the, I don’t know the obvious that continuous glucose monitoring is not just for people with type one diabetes is not just for people with type two diabetes and insulin, but with a little bit of help and support, everybody can benefit from this device diabetes, and we should be pushing that. We should be arguing that we should be celebrating that and making that doable and affordable for folks.
Scott K. Johnson: Well, let’s try and let’s try and turn the light on for, for more people who are stuck in dark rooms right now. Right?
Scott K. Johnson: So, you know, we always try and leave with a couple of takeaways for those who, who watch and, and thank you for watching. As someone living with diabetes, one of my big takeaways is the five Ms. That there are things I have always known that really impact my blood glucose management and diabetes management,
Scott K. Johnson: but there are also things like mood and, and timing that are strong factors in all of that as well. And I think we could spend many more episodes even diving deeper into those topics alone. So let us know if that’s something you want to hear.
Scott K. Johnson: And a takeaway that I might offer up for healthcare professionals is that leading people to their own “AH-HA!” moments can really make a big difference. And the way that we teach is, is a powerful, powerful tool we have in education.
Scott K. Johnson: What, what else would you like to add to that? As far as takeaways?
Dr. Bill Polonsky: I guess I just reiterate what you’re saying and say if you’re a diabetes educator, make the effort to innovate with your programs. Think about how you can include cgm. Think about how you could walk away from didactic learning. And it’s our job to make diabetes education meaningful and useful and engaging for folks. And if you’re bored and your patients are bored, something needs to change. I think that to me is the most important thing, and we know all of our educator colleagues want to do this and want to do better.
Dr. Bill Polonsky: And we just think it’s important to encourage innovation, and let’s all get creative and develop something better.
Dr. Susan Guzman: Yeah, and my takeaway would be how powerful it is when you really can make asking questions about your diabetes, happen in a safe place. And you can only do that by really making it explicitly, this is going to be without judgment.
Dr. Susan Guzman: You know, some people that would be willing to show their numbers had 0% time in range. And that requires, you know, you have to feel safe to do that. And so, you know, really taking the judgment out of it, instead of saying good and bad, like paying attention to, you know, just these are choices, they’re numbers to make decisions. And how do you look at those Ms and how they influence your choices so you can be both informed and consider how diabetes fits into your life.
Dr. Bill Polonsky: That’s wonderful, Absolutely.
Scott K. Johnson: Yeah, very well said. Well, with that, I think you get the feeling that we could talk about this on and on and on. I sure would love to do that. But we also want to respect the time that you share with us. We know your lives are busy, and, assuming you’re managing diabetes or helping others manage their diabetes, you’re even extra busy.
Scott K. Johnson: So, with that, we will wrap this episode up, and we hope to see you next time for another interesting discussion. Thank you.
Dr. Bill Polonsky: Thanks.

