Welcome to episode 3 of BDI Briefs! Our aim with BDI Briefs is to take a brief look at important issues about the emotional side of diabetes.
In this short discussion, Scott, Bill, and Susan discuss some good news recently published about the fear of hypoglycemia. I also encourage you to look at more research from the Behavioral Diabetes Institute.
Enjoy! And please let us know what you think and what you’d like to hear more about from BDI.
And remember to subscribe to BDI’s YouTube channel!
Detailed show notes and transcript
Scott K. Johnson: Welcome to BDI Briefs. This is another installment of what we’re working to make a monthly series where we briefly examine important issues about the emotional side of diabetes. Thanks so much for joining us today. I’m here with Dr. Bill Polonsky, President of the Behavioral Diabetes Institute, and Dr. Susan Guzman, Director of Clinical Education at the Behavioral Diabetes Institute.
Scott K. Johnson: Both are world-renowned diabetes psychologists and as always two of my favorite people to talk with. My name is Scott Johnson. I’ve lived with diabetes for a bit over 40 years and have been active in the diabetes social media space for a while as well. With introductions out of the way, Bill, what are we talking about today?
Dr. Bill Polonsky: Well, I want to talk about some good news. One of the things that I enjoy doing most with these opportunities is really scouring the literature and looking at what are people writing about from all over the world. What are the scientific publications that are telling us good things that oftentimes in our busy lives you don’t get to hear about? And it all has to do with the concerns that so many people with diabetes have concerning fear of hypoglycemia.
Dr. Bill Polonsky: What we know is that for many people listening or watching–and I know, Scott, this has been true for you–if you’ve had diabetes long enough, whether you have type 1 diabetes, if you’ve had type 2 diabetes, especially if you have type 2 diabetes and you’re taking insulin, odds are pretty good you’ve gone through times when you are concerned and worried about the possibility that you could go really low and embarrass yourself, perhaps put yourself in danger, etc.
Dr. Bill Polonsky: In fact, we know worries and fears about hypoglycemia are the number one reason why everyone doesn’t have perfect blood sugars. One of the things we know about fear of hypoglycemia, and this is really my first slide, it really has to do with having lost a sense of confidence in yourself and a sense of confidence in your tools and confidence in your own body. And Scott, you can talk about this for yourself as well, and you can see some of the examples on this slide.
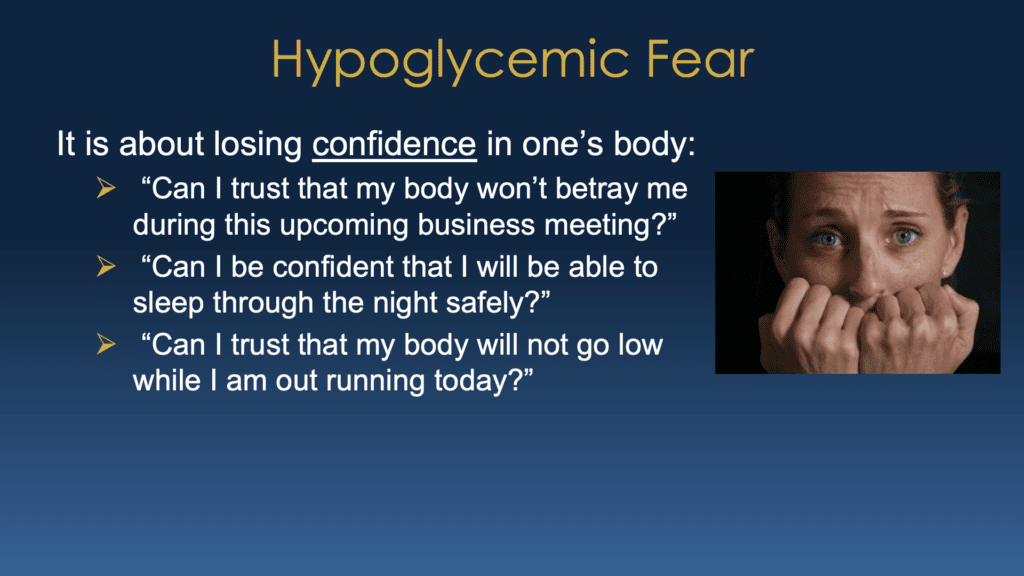
Dr. Bill Polonsky: Can I trust that my body won’t betray me during this upcoming meeting, you know, can I be confident I’m gonna be able to sleep safely through the night? Can I be confident that I won’t go low while running? Or for you, Scott, while you play basketball? And it’s that loss of confidence that really ends up crippling people. So when we think about this, let me just stop and say, Scott, maybe you’d like to talk about your own personal experience. Does that make sense to you?
Scott K. Johnson: Yeah, absolutely, absolutely. And thankfully, I still feel my lows pretty well, even after so many years with diabetes. But regardless, there was a time about a decade ago that I passed out from a low blood sugar in public. And it was very scary for me and for my family. And it really rattled my confidence for a long time. And I know many, many people who have also shared stories of being afraid to be left alone watching their children or they don’t feel they can go run errands by themselves for fear of having a dangerous low blood sugar that they can’t see coming.
Dr. Bill Polonsky: You know, Susan and I have done a lot of work on this, and Susan, I want you to chime in on this. Hopefully, we will have an article coming out later this year where we talk at length about what we understand about what’s going on for people who really have profound fears of hypoglycemia, where it’s really wrecking their lives, and how can we help them? And we look at some things that contribute to the fear of hypoglycemia. There’s actually a long list. But really, some of the biggest ones are the ones you see listed on this slide.
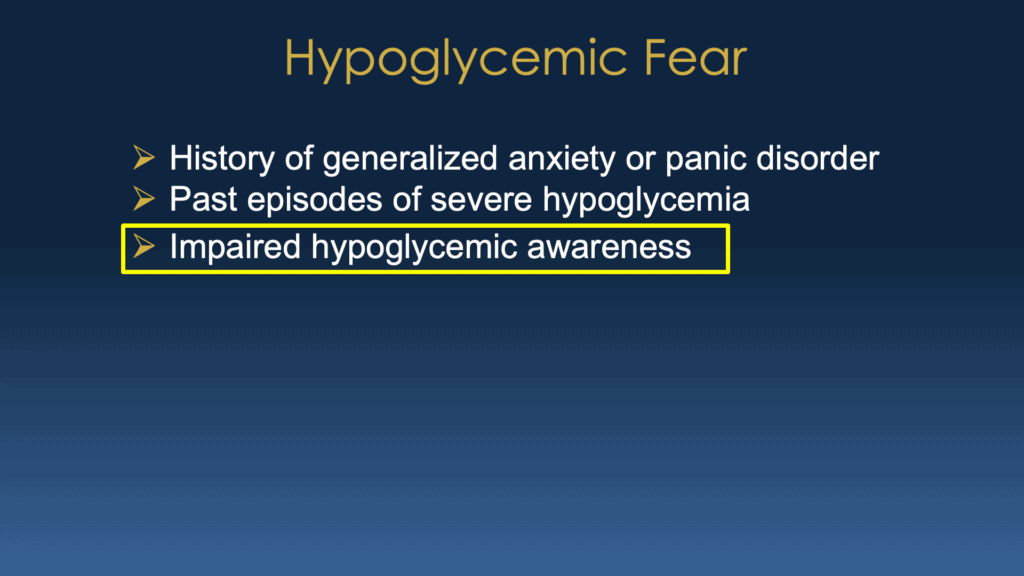
Dr. Bill Polonsky: We know that if you already have a history of anxiety or panic disorder about anything, it kind of puts you at extra risk of also having a lot of anxiety and fear about hypoglycemia. We also know that if you’ve had severe episodes in the past, just like you described, Scott, you don’t have to have a lot. Just one bad episode can be enough to really almost be like a post-traumatic stress disorder. And also we know, there’s a problem with what we call impaired awareness of hypoglycemia. The bottom line is if you’re not having those old warning signs that you’re going low, that also is a big concern. Susan, do you want to say anything else about that?
Dr. Susan Guzman: Well, one of the most exciting things I feel like that’s coming from what you’re going to share is just even the concept that having a decreased ability to feel your lows is reversible for a lot of people. And in fact, when I was first starting in diabetes, they called it hypoglycemia unawareness. And now the name has changed. And I know Bill will talk more about that, that we don’t say unawareness anymore. Because there’s a lot of hope for that problem.
Dr. Bill Polonsky: Yeah, and that’s true. And Scott, I don’t know if this is true. When you were diagnosed, we know most people have had type one, in particular for a long time, are often told, you know, there’s going to be a point where you might lose those early warning signs that you’re going low. And often, those early warning signs are things like, I feel shaky, sweaty, heart palpitation, things like that. They’re called, well, they have different names, adrenergic or neurogenic signs. And that oftentimes those can dissipate and seemingly go away for so many people and you’ve been told that oh that just happens and if that diabetes a long time it’s just not even reversible. Well we know actually it is reversible now and we also know something else that’s really important. Here’s the good news. I want to tell you about this study.
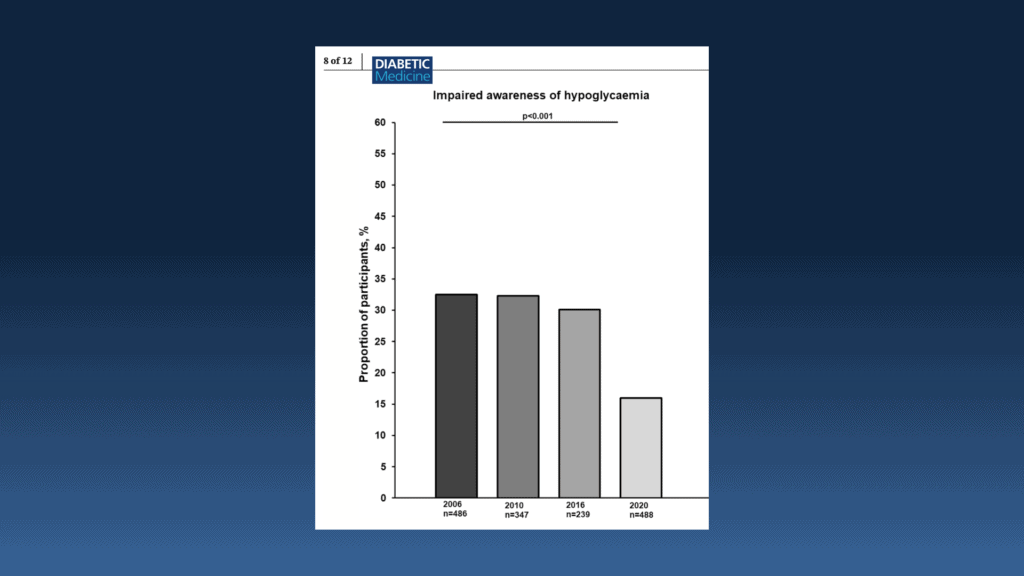
Dr. Bill Polonsky: It was actually just published a couple of months ago. It came from a university in the Netherlands, and in this study what they did is they were able to look at people with type 1 diabetes in their clinic over the course of many years. And they looked at them back in 2006, they looked at them back in 2010, they looked at them back in 2016, and then in 2020. And what they did is they looked at, at each of those time points, what percentage of people with type 1 diabetes had impaired awareness of hypoglycemia. They used this very well-known questionnaire called the Clarke questionnaire. And what they found, if you look at, see from this slide in the first three points, if you look at 2006 and 2010 and 2016, nothing really changed. They were showing what actually Susan and I have seen over the years, which is that a whole lot of people, usually about 30%, of all the people with type 1 diabetes ever seen have impaired awareness, which would put them, of course, at risk for lows.
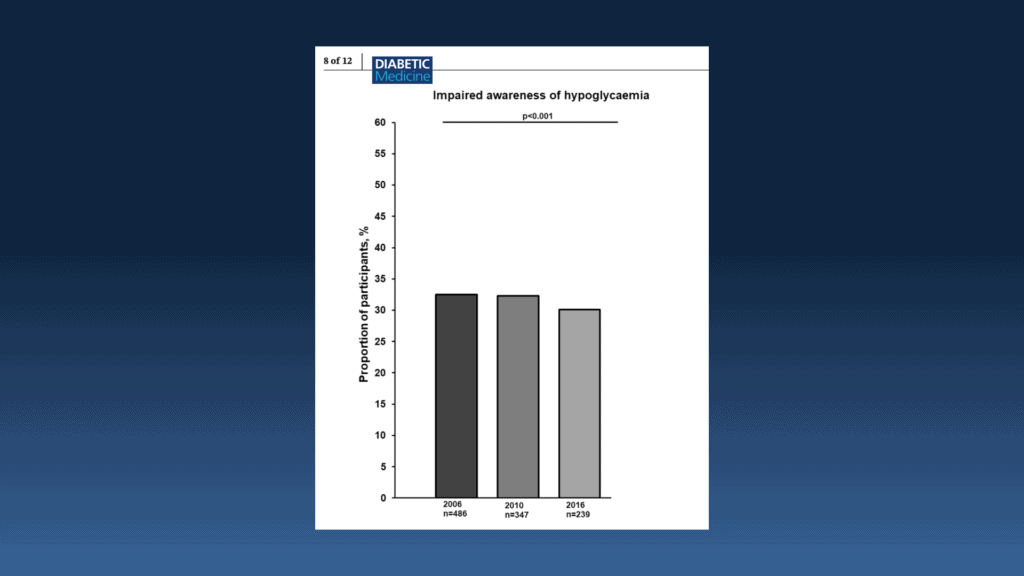
Dr. Bill Polonsky: But here’s what they found when they looked at their most recent sample, which is 2020. And you can see that bar is a lot, lot lower. In fact, it’s half the size of the other bars. And this is the good news that we’re seeing from this clinic in the Netherlands but has also now been reported in several other countries, all within the past year. Which is that the percentage of people with type 1 who have impaired awareness of hypoglycemia seems to have been cut in half. Now, that’s extraordinary. Hasn’t gone to zero, but it’s been cut in half.
Dr. Bill Polonsky: And when you look at why, it has to do with how we, well, we think we know what it has to do with, that we know that impaired awareness can be reversed when people practice going through short periods of time of having few lows or no lows at all. And their symptoms, their awareness of their symptoms begins to come back, those actual physical symptoms begin to come back.
Dr. Bill Polonsky: And so the idea is, actually, because of all our new technology – great CGMs, great pumps, now we have hybrid closed loop pumps, people are actually having fewer lows and because of that they’re beginning to regain their awareness or if we look at people who have had diagnosed in the past few years they may never even have a problem with this. So again it’s not a perfect story and I know Susan’s going to be careful about letting us know we shouldn’t be totally optimistic, but my hunch is as we see continued improvements, as more and more people have access to CGM, more and more people have access to the newest technology, and as that technology is getting even better, that percentage of people with impaired awareness is going to drop and drop and drop and drop.
Dr. Bill Polonsky: And that gives us some really extraordinary hope about how we can help people regain their lives to not have to walk around and be so scared and nervous all the time. So I throw it back to you guys. What do you think of this?
Scott K. Johnson: I definitely agree that one of the biggest things that I’ve noticed since starting on, on some of these new technologies, so CGM and any of the automated insulin delivery tools that are available. I have fewer lows, and the lows that I have are milder and easier to treat and deal with. So it’s easy to see that my body gets used to not being low and therefore I feel the symptoms very early, and it’s a welcome change. I love that about these systems.
Dr. Susan Guzman: I was thinking, you know, since this is such important good news that really it’s important to ask people, do you feel your lows? What’s your experience, Scott? Are you asked in your clinical setting whether you feel your lows? Because if you don’t, there’s good news, right? And maybe people aren’t hearing that news.
Scott K. Johnson: Yeah, that’s a great question. And yeah, so I see my endocrinologist two or three times a year, as well I was just in for my annual physical. My endocrinologist asks about lows, which I expect – he’s my diabetes specialist. But my general physician also asked about low blood sugars, and I thought that was pretty nice as well.
Dr. Bill Polonsky: That’s a good point. So for those of you who have type 1 diabetes or type 2 diabetes and taking insulin and you’re really worried about those and you’re having trouble feeling your lows, you should make sure this comes up next time you see your primary care provider or your diabetes specialist. If they don’t ask you, you should volunteer it. If you’re having trouble feeling your lows and you’re concerned about it, bring it up.
Dr. Bill Polonsky: And by the way, if you’re a provider, you know, they’re busy, they may have to know lots of things, they may not be reading all the literature. If they say, “well, you know, I’m sorry, you’re having trouble feeling lows, that just happens to people. Not much you can do about it.” You could say, excuse me, have you read the recent publication by Ali 2023, recently published in Diabetic Medicine? So again, we want to help busy providers, who can’t read everything, to know that there are these messages of hope that things are changing, and we want everyone to know and to take advantage of these things.
Scott K. Johnson: When we step back and we start to think about takeaways, right? One big message that I get from this is there is hope that impaired awareness of hypoglycemia is reversible, that things can be better if that’s something that you struggle with. And there are tools and support and education available for you. What else might you two add to that?
Dr. Susan Guzman: I would just add what we just said. If you haven’t been asked, make sure you bring it up with your doctor if you’re a person with diabetes. If you’re a clinician watching, it’s one of those things that you can do a lot about. It’s important to address it.
Dr. Bill Polonsky: And again, we want to be careful about a couple of things. Number one, we’re seeing this improvement. Again, it’s, we haven’t taken it from 30% to zero. So it’s not like things are perfect, but we’re seeing things moving in the right direction. And there are other things that can contribute to why people are having trouble feeling their lows.
Dr. Bill Polonsky: But again, it’s by bringing it up, this is something you can talk about with your physician and look at how other medications you may be taking contribute to impaired awareness, et cetera. All things that can be addressed and changed. We know that many, if not most people, can really do better. So if we can help people improve their quality of life just by addressing this one issue, it’s pretty great.
Scott K. Johnson: Yeah, I definitely agree. It’s pretty great and especially for those people who are living in a lot of fear around this – that can be really debilitating. Knowing that there’s hope and change is possible, I think that is a great positive message. So thank you for highlighting that. Anything else that we want to add before we wrap this episode up?
Dr. Bill Polonsky: I think that’s good enough for now. We want to keep things brief and powerful.
Scott K. Johnson: Sounds good. Well, thank you all for watching. Thanks so much for sharing some time with us today. Please let us know if you have any questions or want us to take a look at anything in particular. Leave us some feedback, and we will do our best to do that. And until next time, stay well.