Welcome to another episode of BDI Briefs! Our aim with BDI Briefs is to take a brief look at important issues about the emotional side of diabetes.
In this short discussion, Scott, Bill, and Susan discuss how diabetes has an image problem and why it’s important to discuss evidence-based hope in diabetes.
Enjoy! And please let us know what you think and what you’d like to hear more about.
And remember to subscribe to BDI’s YouTube channel!
Detailed show notes and transcript
Scott K. Johnson: Welcome to BDI Briefs. This is another exciting installment where we take a brief look at important issues about the emotional side of living with diabetes and working in diabetes. Thanks for joining us today. I’m here with Dr. Bill Polonsky, President of the Behavioral Diabetes Institute, and Dr. Susan Guzman, Director of Clinical Education at the Behavioral Diabetes Institute. Both are world-renowned diabetes psychologists and two of my top picks for people to spend time with.
My name is Scott Johnson. I’ve lived with diabetes for over 40 years, and I’ve been active in the diabetes social media space and industry for a long time. With introductions out of the way, Bill, what are we talking about today?
Bill Polonsky: We are going to talk about one of our favorite subjects here at BDI, which is the concern we have about how many people we meet every day with type 1 and type 2 diabetes who are just so discouraged and beaten down because they feel kind of hopeless that diabetes is going to cut their life short or terrible things will happen to them. And we want to talk about that.
We know that actually sometimes, being told that you know you’re at risk for complications actually can help people get motivated or stay motivated to pay attention to diabetes. But we know for way too many people, all those scary messages over time lead to people feeling paralyzed with despair and fear. And we don’t think that has to be true.
And so what we like to do here at BDI is we talk about how we can, well, invert all those scary messages and talk about what we call evidence-based hope. And to introduce that, you know, for those of you who might be watching this saying, well, I don’t have diabetes. Well, why would people get so freaked out or worried about complications?
And it might be because they’ve seen, well, just looking at our first image here, perhaps they’ve seen things like this:
Bill Polonsky: Maybe they saw this in a magazine or on television, “diabetes is a leading cause of kidney failure.” Or maybe they’ve seen something like, you know, blindness:
Bill Polonsky: “Diabetes is a leading cause of new cases of blindness among adults in these age groups,” etc. And we know that when people hear these messages, it matters.
And here is data from our own studies that show, not to belabor everything you see on the slide, but what we know is the majority of people both with type 1 and type 2 diabetes report that, to some significant degree, they do feel kind of doomed, that they’re going to end up with serious long-term complications no matter what they do.

Bill Polonsky: And of course, if that was true, we can understand why people would just say, well, “why would I bother managing?”
So let me stop and ask you guys, what about your experiences, your thoughts about this? We’re next going to talk about some solutions to this, but I just thought we’d stop and say, does this sound familiar?
Scott K. Johnson: I’ve seen messages like this for a very long time. And I think feeling paralyzed is a very good description of it. Because you see a headline like that where diabetes is the leading cause of XYZ, and it’s very often part of a campaign that is surrounded by other information that’s meant to help or perhaps motivate in some way, maybe scare me into action. But so often, I don’t… I don’t see past that scary headline.
Susan Guzman: Yeah, and in fact, in all of our programs at BDI, we hear that as a theme, Scott, that paralyzed, disengaged feeling, because, if what I do doesn’t matter anyway, why should I go to a diabetes education program or attend a diabetes health event or learn more about my diabetes or even bother taking that medication? What’s the point?
So these scare tactics can help. They’re meant to raise awareness and perhaps sell products or raise attention or dollars. But for people with diabetes, beyond just knowing the risks, oftentimes, these tactics backfire. They do often lead people to feel hopeless and that their efforts don’t really matter.
Bill Polonsky: So we think we can do better. And one of the most important ways in which we can do better is–and Susan and I have been presenting this kind of information to groups of folks with diabetes around the world for many decades–to really show that this is not exactly true.
It’s not diabetes per se that is the culprit. It really is the degree to which one is managing their diabetes that could either be leading to potentially problematic or not-so-problematic outcomes.
This is really spearheaded by work we did many years ago with a well-known endocrinologist at the Joslin Diabetes Center in Boston, our dear friend, Dr. Richard Jackson. And I always like to give him kudos for this because he’s really helped us so much in beginning to think about this.
So when we present this to groups, here’s what we do. And so, let’s start by talking a bit about type 1. And we have endless amounts of data we could show that would overwhelm everybody. But I’m gonna show you our favorite two slides. And… This is about what happens to people with type 1 diabetes who’ve been living with this disease for, let’s say, 30 years. In fact, I just showed this to someone I was working with earlier today. And we know that there are large healthcare centers that do a pretty good job helping their patients manage diabetes, and they’ve been collecting this sort of information.
So here’s one group. This is actually from the Steno Diabetes Center in Copenhagen. And they looked at their patient population. Again, people with type 1 diabetes who have had it for about 30 years. And they said, how many of these folks, what percentage of these folks have run into the scary, scary complications that we all tend to think about and lead to people being discouraged? So this is what they found:
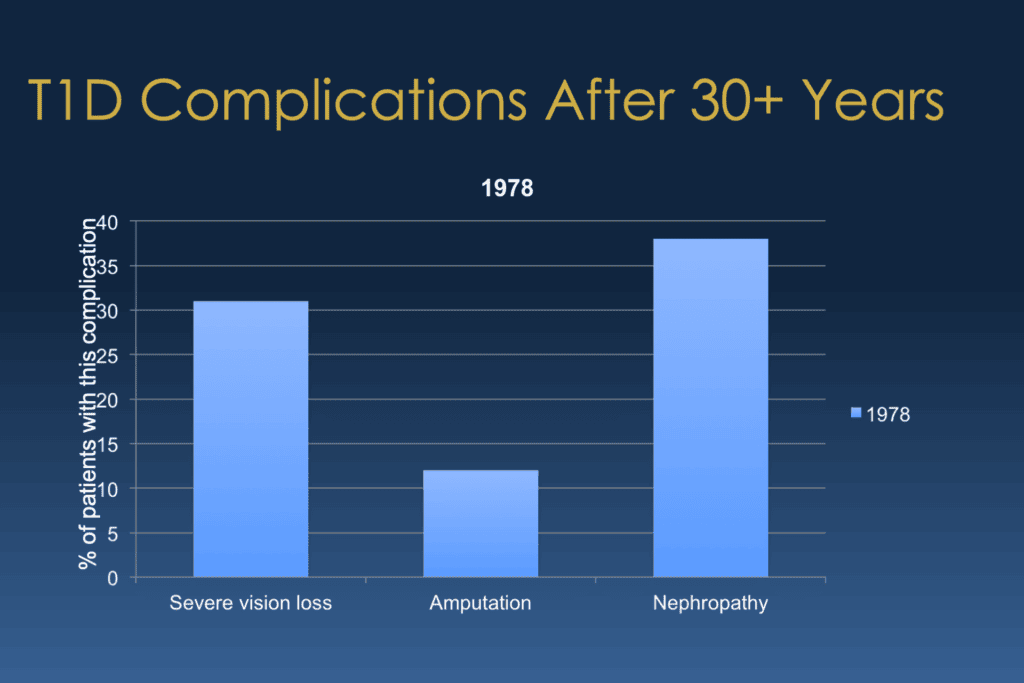
Bill Polonsky: And starting on the left side of your screen, they found that about 30% of this population already had significant vision loss, severe vision loss, or gone blind. that middle column, they found about 12% already had quite significant amputations. And over there on the right, what we call nephropathy, which is kidney disease, that well more than a third, almost 40%, already had nephropathy. And when we show this, and Susan, I’m sure, can tell you this, she sees the same thing, we find that most large groups of folks with type 1 will go, yeah, I’m not too surprised. That’s about what I would have expected.
But if I leave this up long enough, someone will say, hey, why does that say 1978? And I go, oh yeah, forgot to tell you something. This is really, really old data. This was published in 1978. This was a time when there was no such thing as self-monitoring of blood glucose, much less continuous glucose monitoring. We didn’t have analog insulins. We actually didn’t have any convincing evidence that trying to manage your blood sugars mattered anyway. So let’s put this aside and say, well, what about… the 21st century.
And so we turn to a study called the EDIC trial, where they’ve been following another large group of folks with type 1 diabetes for 30 years, but it’s the 21st century now, not back in 1978. And we can ask the same question, which is, well, what percentage of those people here in the 21st century, in this nice program, where they had regular follow-up care for all these decades, had run into the same scary complications? Well, their numbers look like this:
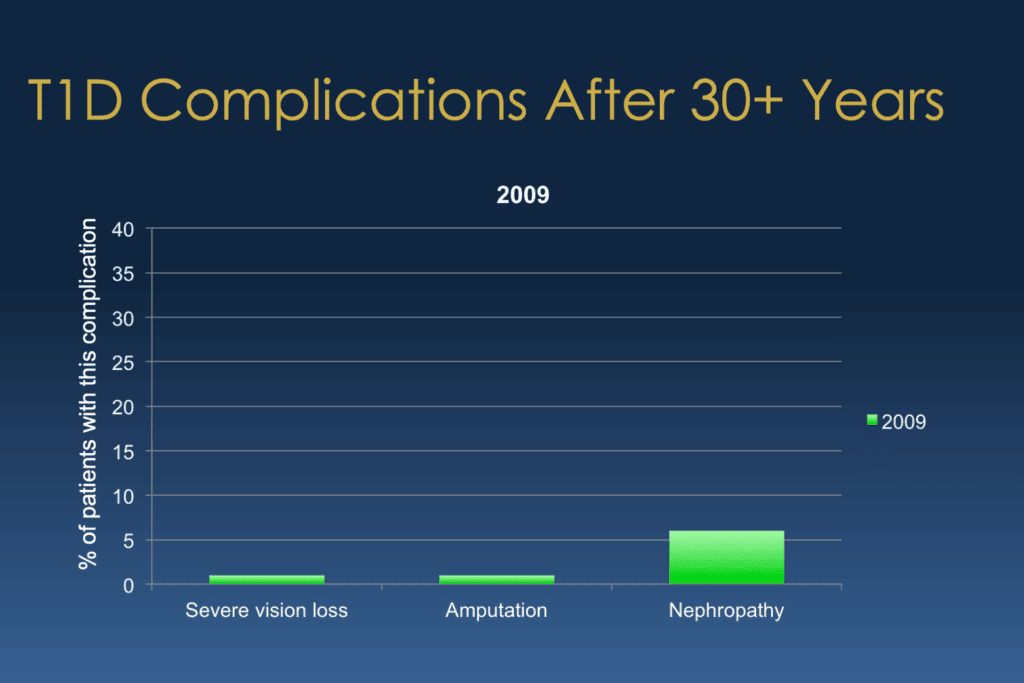
Bill Polonsky: And whenever we show this to groups of folks, everybody just gasps going, whoa, because yeah, you should gasp!
So in this group of folks, it wasn’t 30% of the severe vision loss. It was 1%. And amputation was 1%, not 12. And nephropathy was, again 5%, 6%, not 40%. And this is really, really important. And I want to be careful. We’re not saying, so this is the truth. This is what’s going to happen to you. But we want people to know that This is what’s possible, that things have really, really changed.
By the way, this was published in 2009. We didn’t have very good CGMs. We didn’t have hybrid closed-loop systems. So you might expect if we could redo this tomorrow, things might look even better. But let me stop, Scott. You’ve been living with type 1 for 40 years. Susan, you talk about this with your patients all the time. What do you think?
Scott K. Johnson: I mean, it certainly makes me feel like the future is bright and that the things that I’m doing and working so hard on are making a difference and do matter.
And it also makes me think like, OK, 2009 minus 30 years, that the things people were doing 30 years ago were making a difference and that it’s important for us to continue learning about new things and keeping up with the latest in diabetes because it’s it clearly is making a difference.
Susan Guzman:
Now I think the other really important and hopeful part of this slide’s message is that these folks who participated did not have “perfect” blood glucose management. And they’re, correct me if I’m wrong, Bill, I think that the average A1C of the people that participated in the study ended up being around at 8.2. And so, you know, that’s also… an important piece of the story that you don’t have to be perfect to have good outcomes.
I feel like that’s also another part of the script around how we talk about managing diabetes over time that gets left out because, you know people feel like there are two speeds–at target or not controlled or uncontrolled. You know, “good” or “bad” and that’s an outdated concept, and there’s evidence to show that.
Scott K. Johnson: If I can bring up just one more quick point,
Bill Polonsky: Oh, sure.
Scott K. Johnson: It’s that I also think about, you know, diabetes has improved, but also the treatments for any of these complications that we may bump into have also advanced as well. So even if I do bump into a complication, there’s hope for that complication alongside my diabetes as well.
Susan Guzman: That’s right.
Bill Polonsky: Absolutely. And again, you can see why we like to refer to this as evidence-based hope. We’re not just talking positively here. We’re saying this is what we have data that really supports this idea that we want people to remember things have changed and that it’s possible, you know, with good care and effort, you can live a long and healthy life with diabetes.
Now, by the way, some of you may be watching this thing thinking, well, I have type 2 diabetes. Who cares about type 1? Can we talk about anything similar with type 2? And yes, we can. So I have just a little more data to show you, and then I promise I won’t do too much more, but this is really gonna be it.
So here’s type 2 diabetes. Here’s a recent study; there’s only one study, and it comes from Sweden. And what they did is they looked at everybody with type 2 diabetes in Sweden. They can do that because they have these big national registries. There are about a quarter million people. And they said, let’s compare those people with type 2 diabetes to a similar group. Similar age, similar kind of folks, but they didn’t have type 2 diabetes. And they started at about age 60 or so, and they said, let’s look what happens to those people over about a six-year period. And they looked at a number of different outcomes, but I want to highlight one of the ones we might worry about the most, especially with type 2 diabetes, which is running into significant heart problems or having a first heart attack. So here’s what they found in this study:
Bill Polonsky: So first of all, what you see is that little blue column on the left, and don’t worry about what you see on that y-axis on the far left. But basically, what we’re showing here are sort of the percentage of people in this study who didn’t have type 2 diabetes, who had a first heart attack over this period of time when they were paying attention, following people over these years. And then you look at people with type 2 diabetes, and this is what they found:
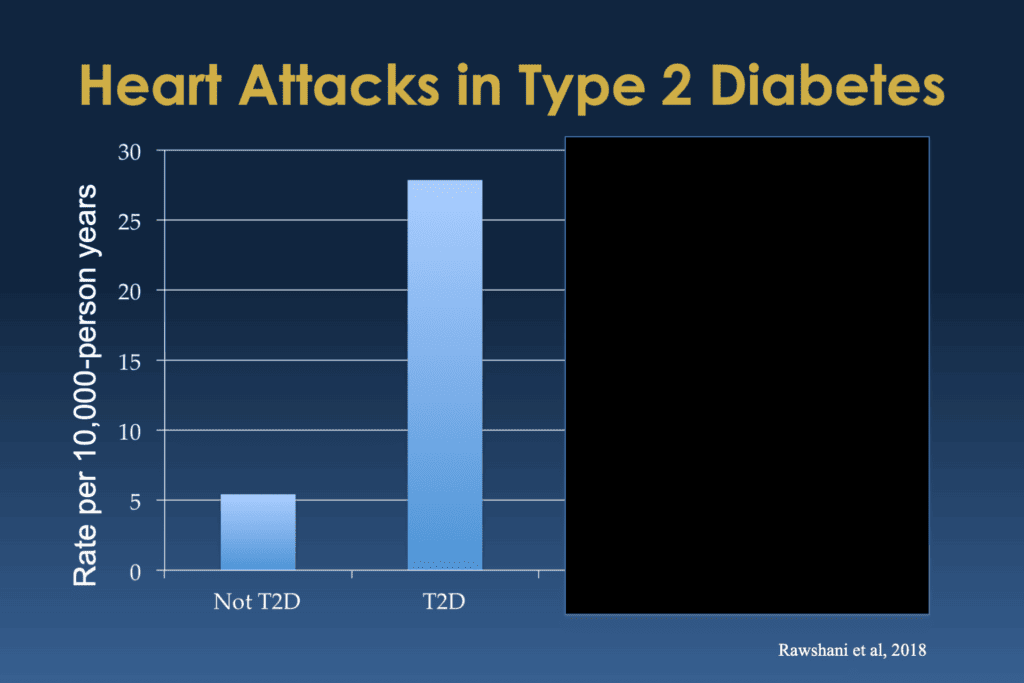
Bill Polonsky: And you can see that people with type 2 diabetes had way higher risk and way higher percentage of them ran into heart attacks. In fact, it was more than quadruple the risk.
So again, when I show this to folks with type 2 diabetes, they go, yeah, I’ve heard that people with diabetes, especially type 2, a much higher risk for heart problems.
But then I admit I’m lying, actually, and that big giant column actually isn’t people with type 2 diabetes. It’s actually people with type 2 diabetes who also have five significant risk factors.
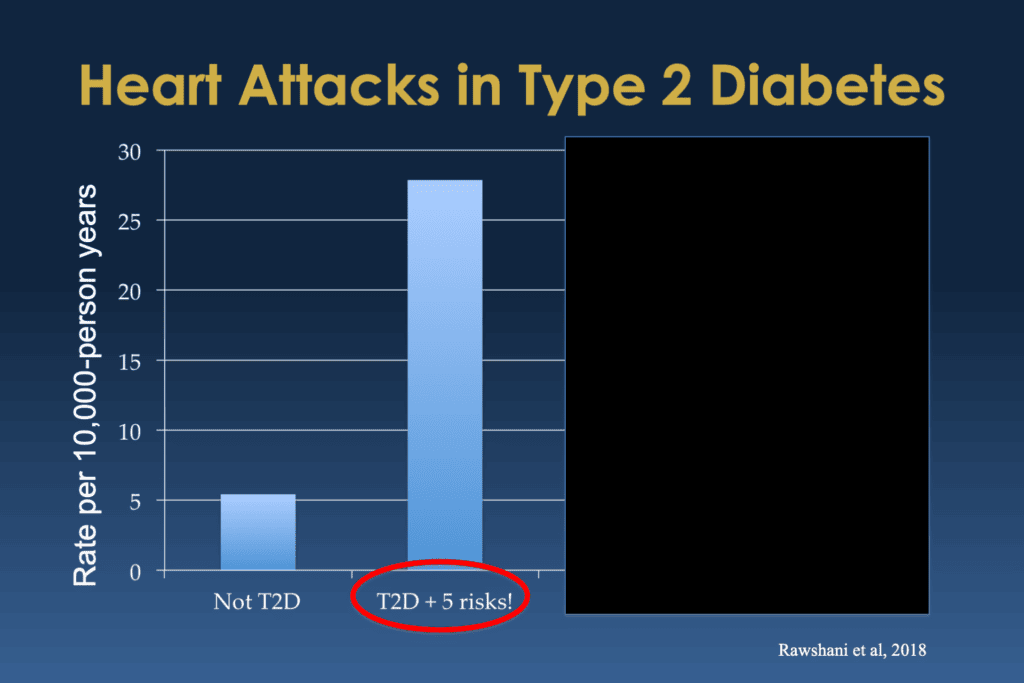
Bill Polonsky: So they have elevated blood sugars, they have elevated blood pressure, they have elevated cholesterol, they have elevated what’s called albuminuria, which is early kidney problems, and they’re smokers. So yeah, you add up all that, you can see why they’d be a much higher risk for heart problems, having a first heart attack.
But what about people who have type 2 diabetes and have pretty good care and they don’t have any of those elevated numbers and they’re not smokers?
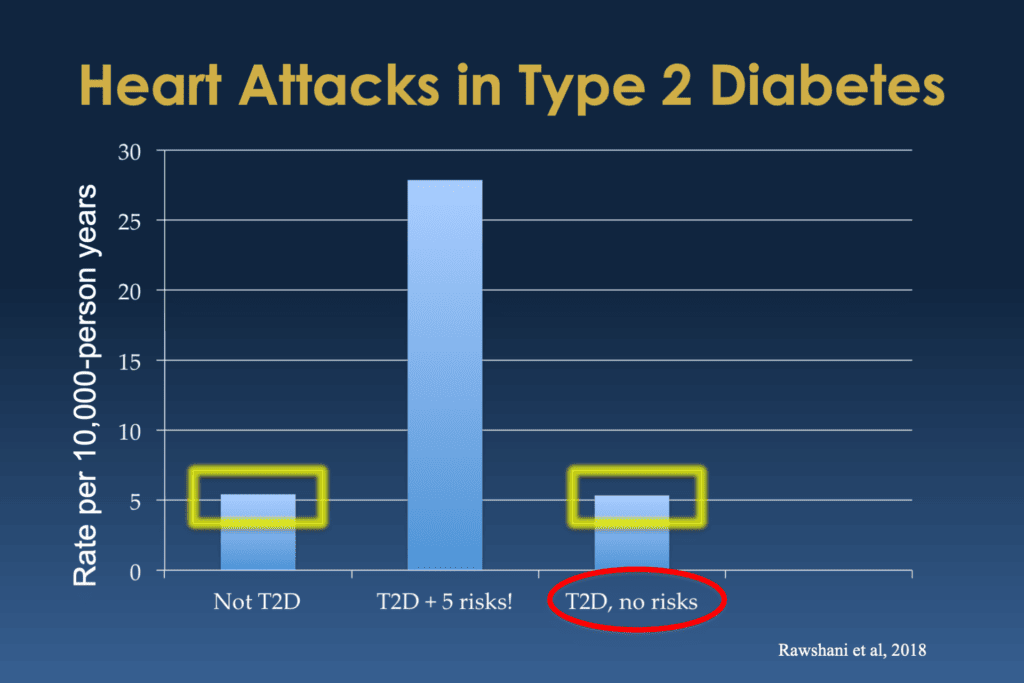
Bill Polonsky: Well, the percentage of them who had first heart attacks was over there on the far right. That’s it.
Now you might notice that column looks a lot like that column of people with type 2 diabetes. Actually, it’s a little lower. In this study, the people with type 2 diabetes who didn’t have any of those extra risk factors, they’re likely to have had their first heart attack was less than people who didn’t have diabetes.
So again, it’s only one study. I don’t want to overstate it, but the purpose of this is to say this is what’s possible. With good care, decent care, odds are pretty good, you can do well. And again, live a long and healthy life. So, evidence-based hope. Guys, what do you think?
Scott K. Johnson: I mean, that looks wonderful to me. It really made me smile looking at the type 2 diabetes plus no additional risks being the same or even, as you mentioned, a little lower than without type 2 diabetes. That’s amazing.
Susan Guzman: Yeah, and in the interest of time, we didn’t include all of the data, but we’re not just talking about no risks, because even if you have fewer risks, that line goes down. So even if you don’t smoke, for example, one fewer risk factor, and your risk goes down. So every one of those five risk factors that you can take off, it matters.
Bill Polonsky: Every single one counted, absolutely. Yeah, your efforts can make a big difference.
To be fair, the last point I want to mention about this is that even though we’re having, and this is just a little bit of the data that’s out there showing us that the idea of evidence-based hope is reasonable. What’s unfortunate is that we’re still hearing these often discouraging and deflating messages.
So the news about specifically significant cardiac problems, heart attacks, for example, people with diabetes, especially type 2 diabetes, over the past decade. This is very similar. It looks really, really good. Except how does that data get presented to people with diabetes? How does that data, that good news, get presented to healthcare professionals? Well, here’s my favorite. This is from what’s called Diabetes Pro. It comes to almost everybody who’s a healthcare professional in the field. And this was the announcement. You ready? The announcement is, guess what?
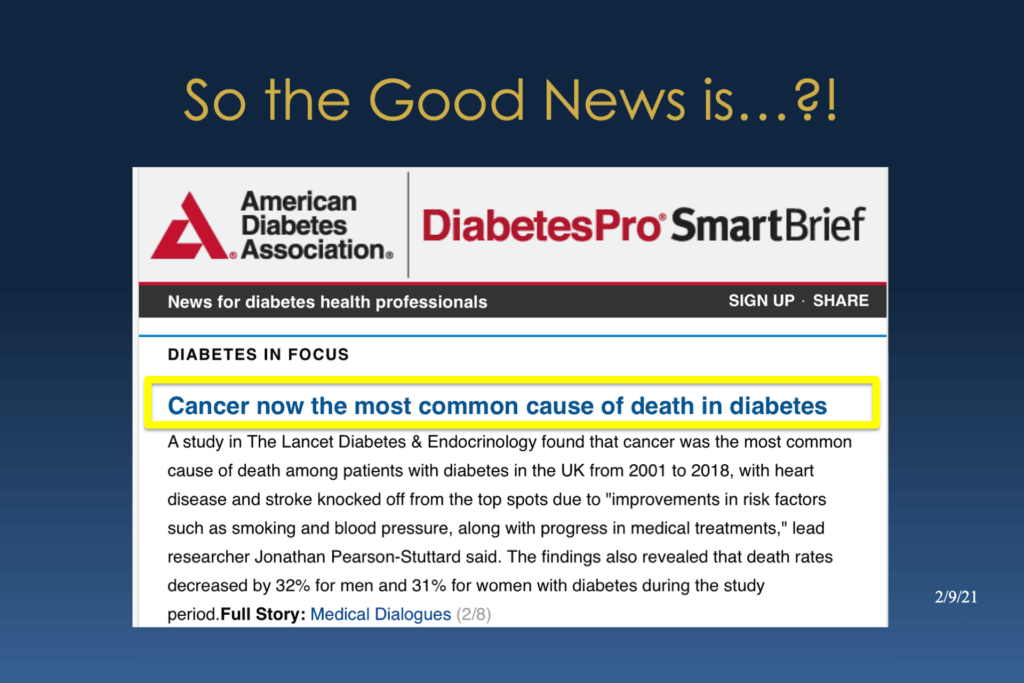
Bill Polonsky: Cancer, now the most common cause of death in diabetes.
Well, actually, if you read the rest of this, the reason that’s now true is because people aren’t dying of heart disease. That there’s been such a profound improvement in people dying from heart disease who have diabetes, that what do we got left? You know, well, cancer, something we should all be concerned about.
But is this how we want to share this news with folks? I mean, we can always go for the negative, but there is this evidence-based, hopeful, positive message that sometimes gets missed. I just find this so funny. Guys, what do you think?
Scott K. Johnson: There’s a clear need for shows just like this, right? Where we can shine some light on these types of topics without a headline like that.
Susan Guzman: I think it really shows how diabetes has an image problem.
Bill Polonsky: Well put.
Susan Guzman: We in the field seem determined to highlight the good news in diabetes by focusing on the negative. I really feel like we do need a culture shift in diabetes, an image change.
Bill Polonsky: Yeah, here here. That’s pretty much all we really wanted to talk about.
We don’t want to belabor this point, but I’m hoping those of you who are watching will pay attention for other potential good news. Again, we don’t want to pretend there isn’t bad news. We don’t want to pretend that bad things don’t happen.
But what we know is that things are getting better and that with good care and with effort, the odds are better and better and better that you can do well. And I think everybody with diabetes in this country, in this world, needs to know about this.
I hope you’ll share the good news.

