In this episode of BDI Briefs, we dive into causes, symptoms, and strategies for managing fear of hypoglycemia for people with type 1 and type 2 diabetes.
Learn about the Be Safe and Feel Safe strategies, the importance of diabetes technology, and how to regain confidence in blood sugar management.
Polonsky, W. H., Guzman, S. J., & Fisher, L. (2023). The Hypoglycemic Fear Syndrome: Understanding and Addressing This Common Clinical Problem in Adults With Diabetes. Clinical diabetes : a publication of the American Diabetes Association, 41(4), 502–509. https://doi.org/10.2337/cd22-0131
Detailed show notes and transcript
Scott K. Johnson: Welcome to BDI Briefs, where we take a brief look at important issues about the emotional side of diabetes. Thanks so much for joining us today. I’m here with Dr. Bill Polonsky, President of the Behavioral Diabetes Institute, and Dr. Susan Guzman, Director of Clinical Education at the Behavioral Diabetes Institute.
Both are world-renowned diabetes psychologists and two people I’m very glad to have on my side as I navigate life with diabetes. My name is Scott Johnson. I’ve lived with diabetes for over 40 years and have been active in the diabetes social media space and industry for a long time. And with introductions out of the way, what are we talking about today?
Dr. William Polonsky: Well, thanks, Scott. You know, like we’ve done in previous programs, I’ve tried to search the literature and say, I’m going to find some new publication that really seems important, both for health care providers working in diabetes and also just regular folks living every day with diabetes. And so I found this really amazing article, it’s about what’s called the hypoglycemic fear syndrome, and was written by some really impressive authors.
Dr. William Polonsky: Oh wait, that’s us. So this is an article that Susan and I wrote with our colleague Dr. Larry Fisher. Professor Fisher is from the University of California, San Francisco, and it’s a subject that’s near and dear to our hearts because Susan and I have done some very long, all-day-long programs and workshops for healthcare providers to help them be informed on this topic.
So just to set the stage, and Susan, I want you to chime in, Scott, you’re going to chime in because I’m sure you’re very aware of this topic. We want to talk about, well, fear of hypoglycemia. We know that it’s really normal for people with type 1 diabetes and for lots and lots of people with type 2 diabetes to be uncomfortable and worry that you know, hypoglycemia could harm them, can make them uncomfortable. But in this article, we wanted to focus on a subset of those, and it’s what we call the hypoglycemic fear syndrome. And these are people who have not just a little bit of concern and fear about hypoglycemia but have a lot of fears.
Dr. William Polonsky: In fact, those fears are so strong that they tend to keep their blood sugars too high all the time because they’re so freaked out about the fact that they might go low and something bad could happen. And what’s really quite remarkable about this is even though I can tell you for a fact that there have been publications and studies looking at the problem of fear of hypoglycemia for more than 35 years, what’s funny is that there’s very little written about what to do about it, which is really striking.
Dr. William Polonsky: I continue to be surprised. There was a great article, not too many years ago, written by one of our colleagues in Canada named Michael Vallis, who actually wrote a lovely article saying, well, you know, here’s how we think about what can be done, how to address really profound fear of hypoglycemia.
And it really struck me that, well, wait a minute, we do this all the time. We should be taking a look at what we do. So Susan and I, in collaboration with Larry, sat down and said, let’s try to bring it all together, citing what literature we can, also looking at our own experiences. So I don’t know; before I say anything more about that, Susan, do you wanna chime in about this?
Dr. Susan Guzman: Well, I think that pulling from the paper, the most important thing to focus on is how we’ve structured it based on the two ways that we are encouraging people to take a look at this challenge, which is ways to be safe and ways to feel safe. And I think they’re– while that may sound like they should be the same things, they’re not.
Well, there’s some overlap, but they’re actually different things to actually literally be safe from hypoglycemia and to feel safe because some people are not at greater risk for hypoglycemia, but they don’t feel safe, and so we, they are, often require separate strategies, so you know, I really encourage people to take a look at both the Be Safe and Feel Safe strategies.
Dr. William Polonsky: Right. And we want to spend all of our time actually going through some of the details of those two sets of strategies, Be Safe and Feel Safe. But Scott, I need you to chime in because I think one of the things that, you know, you offer that I can’t is that you’re living every day with type 1 diabetes.
And this idea that despite the fact that you may have your, you may have all of this together, we know it’s common to have times when you can get kind of freaked out. What do you think? Is there anything you want to mention about that for you?
Scott K. Johnson: Well, just that this definitely hits home for me. In my adult life with diabetes, I have experienced a couple of severe hypoglycemic events where I needed assistance, and it was indeed traumatizing.
It affected me for months afterward. Um, And I also just want to recognize that the safest area for us to walk with diabetes is kind of right next to the cliff, you know, as close to normal as possible doesn’t leave much room for error in that low blood sugar range. So we walk a tricky tightrope.
Dr. William Polonsky: It’s the frying pan or the fire, right? We understand that. And so we know that, oftentimes, just like you experienced, it can be just one bad low. It can be almost like it’s a trauma. And it leads to what almost is sort of a form of post-traumatic stress disorder, where it can reverberate over years, decades even, so that people become so scared, they again, they’re just going to say, “Well, I don’t want to be this scared, so I’ll just ride high all the time.”
And so what we’ve seen over the course of years, and this is what Susan’s talking about, Sometimes what’s going on is that people really are in danger of severe lows, and so our job has to be to say well what do we need to do to help people to be safe. For lots of people, though, it turns out that’s not enough.
Dr. William Polonsky: You can actually help them to be safe or get safer so that the risk of going low is less, but they, they’re still freaked out. And so we have to have separate strategies that look at, can we help people to feel safe? And by the way, sometimes we’ve dealt with folks who actually, physiologically speaking, they are safe.
They’re not really at any risk of going low, but they’re still freaked out. So that’s when we want to focus on our feel safe strategies more. So sometimes we’ll use be safe strategies. Sometimes we’ll talk about feel safe and lots of times we have to do both. So I hope that sets the stage well. Susan, I interrupted you because you were getting into it.
Dr. William Polonsky: So the first set of strategies is what we call be safe strategies to help make sure for someone who’s freaked out that we can help them to take action so that their risk of getting, becoming low is, well, not so bad. And so, again, we, we look at medical interventions, we look at behavioral interventions, but now, Susan, I’m going to turn it over to you.
Let’s walk through some of our Be Safe strategies and there are six of them.
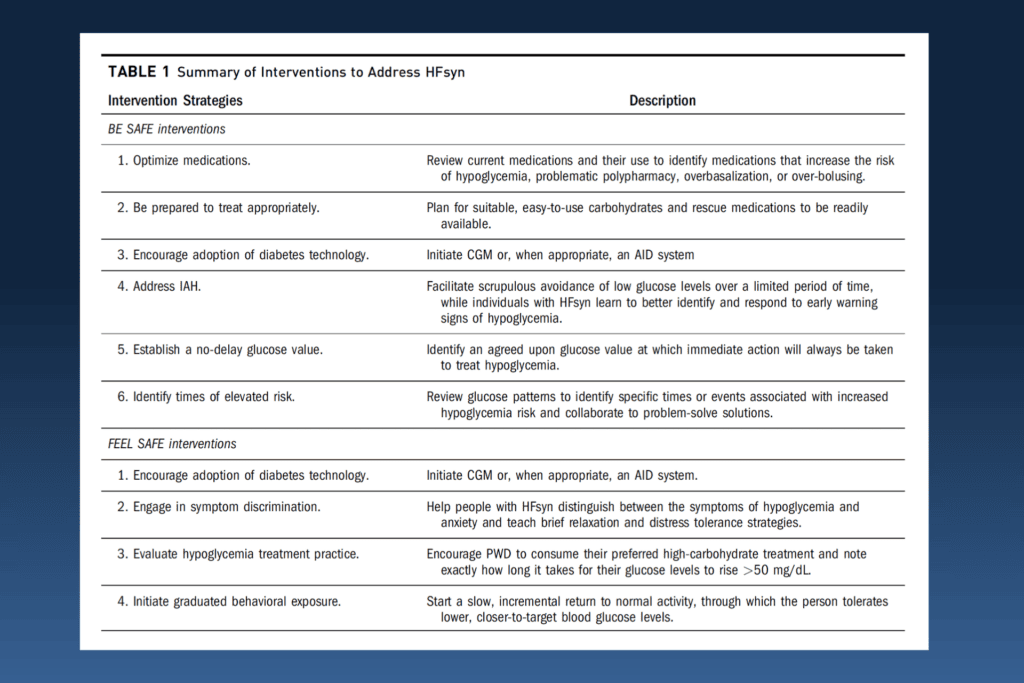
Dr. Susan Guzman: Sure. Well, the first one is to optimize medications. So obviously, if, you know, somebody has their dosage wrong with their basal rates or their correction factors or something like that with insulin, or perhaps they’re on oral medications that not optimized dosage, you know, they’re at more risk for hypoglycemia. Obviously, that would be a great place to start. Then the other thing that I find is a little, a little bit sneaky for people sometimes is the second one, which is to be prepared to treat appropriately.
A lot of times, when people have a low, they choose their treatment with something that isn’t actually a really fast-acting carb. I remember one of our good friends, to BDI said, you know, she hates to waste a, a hypoglycemic treatment on, you know, glucose tablets or something like that when, you know, that’s a good opportunity to eat a candy bar or a cookie and, not have to feel bad about it, but unfortunately, when you select not fast acting carbs, that then, you know, people can have, have some problems from that.
Dr. Susan Guzman: And also sometimes people will think that you know more equals faster. That’s a common experience because, you know, your brain’s saying like a, you know, get out fast. And, people will sometimes think, “Well, I should just keep consuming carbohydrates until I feel better,” which is a normal response when you have that fight or flight going off in your brain.
But unfortunately, more does not equal faster, and then people end up, you know, having a high later that they end up chasing, sometimes followed by another low. I had that happen to one of the people I worked with yesterday. And saw how she chased both directions from that problem.
Scott K. Johnson: That’s a big problem for me. I want also to acknowledge that those feelings when your blood sugar is low, they’re, they’re downright primitive survival. Eat everything you can see. And, it takes incredible discipline to treat a low rationally and then sit on your hands and wait. It’s so hard.
Dr. Susan Guzman: Yeah and that and that isn’t always possible for everyone, and I think that we need to acknowledge that, right?
Dr. William Polonsky: I don’t want to get us distracted about how you could treat your low perfectly. We just want to make sure people are safe and being safe. Like do they even have stuff? I mean how many times over the past 30 years have I met people who said, “Yeah I was out for a run and I started feeling low and I went, oh yeah, I didn’t bring anything with me.”
Are you kidding? So, I mean, little things about, you know, do you have stuff in your glove compartment in your car, you’re prepared. You know, we now live in a different world where we have stable glucagon. You know, we have glucagon you can just puff into your nose. We have glucagon that doesn’t, isn’t one of these fancy kits that you have to like have someone mix all this stuff.
Dr. William Polonsky: Do you have stuff around that can help you or help your loved one help you in the case of an emergency? So these are I hope obvious points But oftentimes we spend a lot of time just making sure these are things that can help people to be safe All right, I interrupt you, Susan. Let’s go on.
Dr. Susan Guzman: Both of you chime in whenever. The other one is probably all of our favorites which is to encourage adoption of diabetes technology continuous glucose monitoring or the new automated insulin delivery pumps. Those are, you know, I think big game changers for people with this challenge.
Dr. William Polonsky: Yeah, I mean, there’s no question, and there have been lots of studies, I’ve been a part of several of them, that have shown just introducing CGM, again, CGM stands for Continuous Glucose Monitoring, especially for people with type 1 diabetes, really can have a quite significant impact on reducing fears about hypoglycemia.
And why wouldn’t it? This is the first time you really know where you are and where you’re headed.
Dr. Susan Guzman: Yeah. And you hear a lot about people describing their challenges feeling their lows. So, addressing impaired awareness of hypoglycemia by helping them pay attention to better identify and respond to the early warning signs of hypoglycemia.
Sometimes people actually get very good at ignoring the symptoms of hypoglycemia. Where they actually think they’re not feeling them, but if they, if they practice tuning in, a lot of people begin to become more aware of the subtle symptoms that they’ve actually practiced sort of pushing through.
Dr. Susan Guzman: I wonder if you’ve had that experience, Scott.
Scott K. Johnson: You know, I don’t think so. I feel like I recognize my lows. But that being said, I’m sure some symptoms happen before the symptoms I’m talking about, and maybe I do push through. Because lows are, are interruptions, right? They’re pulling you away from whatever your attention is focused on.
So I initially said no, but after some more thought, probably so, yeah.
Dr. William Polonsky: And just to highlight, we do meet lots of folks who become very fearful of lows, and again, they have a particularly good reason, which is that they aren’t feeling their lows anymore. And that’s really scary. That’s why CGM is useful.
But also, the reason we have this highlighted on the… on this slide, and this is one of our important strategies, is that we actually know there are steps you can take to begin to restore awareness of hypoglycemia, maybe not completely, but can help people to regain some of those cues. We’re not going to go into details about that, but there’s a whole body of literature about that that we can happily share with people as well. Susan, we got two more.
Dr. Susan Guzman: Yeah, well, well, I, I think probably one of the things that we talk about a lot is just establishing a no delay–and I would add non-negotiable glucose value–that you call hypoglycemia.
So if you have a number, say 70 mg/dL, that you identify as a low, that that’s the number that you agree that no matter what, no matter how inconvenient, no matter how much it’s a problem in the middle of whatever it’s interrupting, that you have a promise to yourself that you’re going not to delay and not negotiate with it, that you’re going to respond to it.
Dr. William Polonsky: Really good point. And again, the last one you want to mention about that as well.
Dr. Susan Guzman: And identifying times of elevated risk, to make sure that people understand like after a, after a severe low, for example, they may be at higher risk for another hypoglycemia event. Also like exercise or people identifying times when they maybe need to pay closer attention or plan ahead. Or like that going out for a hike thing that you used as an example earlier, Bill.
Dr. William Polonsky: So again, all these things, these, these six strategies, and there are more, but we think these are the key ones that can help people actually to be safer. But again, so many of the folks we see struggling with this hypo fear syndrome, it’s not enough.
So that’s when we talk about this other set of strategies we call feel safe. And so those are listed on the slide that you can see, four of them. And the first one, you’re going to say, wait a minute, didn’t we just talk about that? The first one is about, again, encouraging the adoption of our cool new diabetes technology.
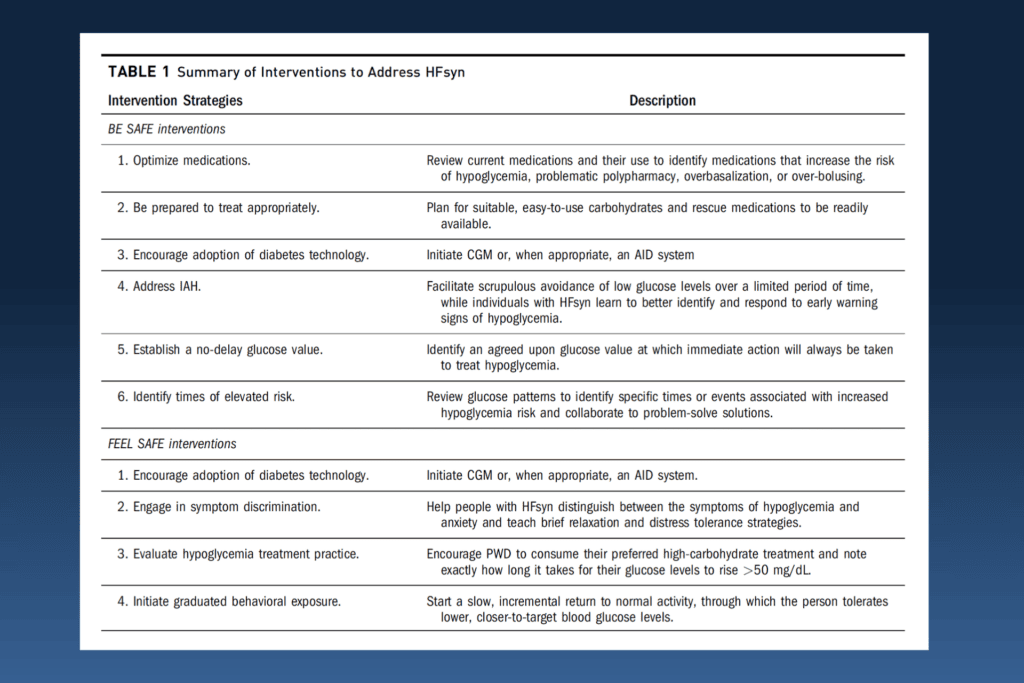
Dr. William Polonsky: We’re especially talking about continuous glucose monitoring. But for those of you who are on insulin, especially if they’re type one, we have what are called automated insulin delivery systems, what are also called hybrid closed loop systems that can really make a difference. Not just in being safer, but again, helping people to feel more confident that they can be okay, that they’re going to be able to catch problems before they happen. And this is why we list it twice, because we see it is so important.
The second one I’ll mention of the four talks about helping people to be clear about what’s called symptom discrimination.
And what this is about is, sometimes when you’re having a low, Scott, I don’t know if it’s ever happened to you. Often, you’re not sure what it is. You know, am I having a low, or am I just feeling weird and funny? The problem is, a lot of what are called neurogenic cues, your adrenal gland shoots off all sorts of interesting hormones when you’re having a low, are the same hormones that are, that are spewed out by your body when you get scared.
Dr. William Polonsky: So we see lots of people who will say, “uh oh, I can feel my heart palpitating, does that mean I’m low? Well now I’m really freaked out, so my heart’s palpitating even more.” And those often get confused. So we have a set of strategies, too much to talk about in detail right here, and we can help people to pull those apart.
Often based on helping people practice simple relaxation exercises as a place to start and to realize that when the feeling is “I’m low, I’m just having this fear response.” So helping people tell the difference is often an important step to helping people to, again, regain that sense of confidence that they can not just be safe but actually feel safe.
I’m going to stop. Susan, what about, want to mention about the last two we have here?
Dr. Susan Guzman: Yeah, that, the hypoglycemia treatment practice. A lot of times, it’s really helpful, you know, Scott, you mentioned that your instincts are not to eat 15 grams of carbs, wait 15 minutes. If you’re still low, eat another 15 grams of carbs.
That’s like a fire alarm going off in your body, in your brain, and you’re saying, get out fast. And so, one way to practice the treatment to help you feel safe is to, is to actually try out your favorite treatment for hypoglycemia when you’re not low. So that you can see, gee, when I have this small glass of juice, it’s gonna take my body about 20, 25 minutes to come up 50 mg/dL.
So you know that that uncomfortable feeling that sit on your hands feeling that you described Scott is going to take that much time, and so it helps you then see that it is an instant and that it does come up, but it does require time So it starts helping people trust that that treatment actually will work when you need it and you practice that when you don’t need it so that you can start to trust you when I have this treatment, it will come up and I’m going to have to tolerate that very unpleasant feeling of being low for, 20, 25 minutes and you get to see that it works. What do you think about that, Scott?
Scott K. Johnson: I love this idea because it’s easy for us living with diabetes to read and learn about how things are supposed to work and this is an opportunity to really match that with personal lived experience, which really goes a long way to building that trust. So I love this idea.
Dr. William Polonsky: Again, I want to underscore this: the idea that helping people gain trust and confidence is really the key to how you address really profound fear of hyperglycemia. People need to know that they can be safe and they can actually feel safe. And that’s why strategy is so important.
Let me chime in and mention the last one, which is about what’s called graduating behavioral exposure. You know, this is really at the heart of what we do when we’re treating an anxiety disorder, many types of anxieties. And that’s really what this is. One of the things we’ve discovered over the years is people who are really struggling with the hypoglycemic fear syndrome in a profound way, there’s often a history of it.
So they’re sort of primed for having these kinds of problems or at risk for this happening, where you have a scary hypoglycemic event that combined with them already being at risk for an anxiety problem.
Dr. William Polonsky: So we put this last, but in truth, I can’t even think of anyone I’ve ever met where we didn’t eventually have to get to this point of saying, now to regain confidence, it’s time to take some risks. It’s time to put yourself in a situation where it’s a little scary and see what these strategies we’ve already talked about.
You can still be safe. So that can mean, “I feel a little funny, can I wait 10 seconds before I, you know, start eating something,” or “can I take the risk of starting to make, go on, you know, take a little more insulin than I typically take, or going for a longer walk than I typically take,” and you sort of build things one step at a time to help people know, and Susan and I both think how successful this is, how people can go, “Oh, it worked, I can do this!”
And that’s why it’s so important, and it really is a linchpin of everything we do. But we put it at the end because we want to make sure all other pieces are in place.
Dr. William Polonsky: Does that make sense? Susan, are you okay with that? Does that make sense? You know, so we put all these together, and we think this is a pretty good place for everyone to be able to start. We want healthcare providers to be aware of this, and of course, we encourage them to go read our article as well, which is published in Clinical Diabetes.
But also to consider these separate interventions that we want to help people to be safe, but be aware that for someone who’s been terrified about lows, that may not be enough, and we have to help people gain confidence and gain trust to feel safe and to understand there’s both of those things that are often needed and how they can work together.
Dr. William Polonsky: So we could belabor this and talk about this all day, but we’ve probably already gone longer than we typically do with our YouTube videos. So, let’s bring this to a close. Any last thoughts, Susan? Scott, what do you think?
Scott K. Johnson: I love the attention on building confidence. That’s such a big piece of living well with diabetes, and that is often what’s kind of swept out from under our legs when we experience a severe hypoglycemic episode, and so rebuilding that confidence, I think it’s really important, and I appreciate the focus on that
Dr. William Polonsky: Susan, what about you?
Dr. Susan Guzman: I guess my final thought is kind of like we’re at the beginning, which is we can’t know people are feeling this way unless we ask.
So, don’t forget to ask people how they’re feeling about hypoglycemia or, you know, how they’re feeling about their confidence in responding to hypoglycemia. I think that just asking that question can really be a turning point for someone who’s had these challenges.
Dr. William Polonsky: It’s a really good point. We want healthcare providers to make sure they ask. How important that is, thank you.
Scott, why don’t you take us home?
Scott K. Johnson: All right. Well, first of all, thank you both for your great work on this and not only for learning more about it and working to understand better what’s going on but also for providing some very practical tactics that can be taught and applied.
I think that that’s really helpful. So thank you both for that. To all of you out there watching and listening, thank you for your attention and we look forward to seeing you again for our next episode.

