Introduction
Welcome to BDI Briefs! In this episode, we dive into the emotional aspects of diabetes. With Dr. Bill Polonsky, President of the Behavioral Diabetes Institute, and Dr. Susan Guzman, Director of Clinical Education at the Behavioral Diabetes Institute, we explore the often-overlooked topic of what happens to individuals when they are first diagnosed with type 2 diabetes.
The Overwhelming Emotional Response
When someone learns they have type 2 diabetes, it can be an incredibly challenging moment. There is often a strong negative emotional response, including fear, worry, and disappointment. People may question their future, wonder how others will perceive them, and worry about what living with diabetes looks like, leading to uncertainty about what the diagnosis means for their lives. These emotional responses, if not addressed, can hinder their ability to create a healthy plan for living well with diabetes.
The Importance of Addressing Emotional Needs
Recent research published by Boakye and her team shed light on how common these emotional responses can be, and the lack of support people receive. As many of you already know, people with diabetes rarely have these feelings acknowledged or discussed with their healthcare providers. They often feel abandoned and unsure about how to proceed. These studies also emphasized the need for healthcare professionals to ask about patients’ feelings, offer support, and answer their questions.
The Role of Healthcare Providers
Healthcare providers have a unique opportunity to make the initial diagnosis experience much more positive. It is crucial to communicate messages of hope, destigmatize the experience, and assure people that the diagnosis is not their fault. Collaborative conversations allow people to express their concerns, ask questions, and establish a partnership with their healthcare team. This approach has proven effective in helping people successfully manage their diabetes over time.
Providing Resources and Support
Just telling people about these important aspects is not enough. It is vital to engage them in conversation and ensure their concerns are addressed. The Behavioral Diabetes Institute developed a resource called the “Don’t Freak Out Booklet” specifically for people newly diagnosed with type 2 diabetes. This booklet provides ten essential tips to navigate this challenging phase, offering evidence-based hope, addressing stigma, and emphasizing that a diabetes diagnosis does not mean a life of deprivation. It is available as a PDF download or as printouts.
Conclusion
Being diagnosed with type 2 diabetes is undoubtedly an overwhelming experience. However, healthcare providers can make a significant difference by acknowledging and addressing the emotional challenges. Engaging in collaborative conversations, offering support, and providing helpful resources can empower people to manage their diabetes and see it is possible to live a long and healthy life with diabetes.
Thanks for joining us today, and remember – you are not alone in your diabetes journey.
Publications
Boakye, M. D. S., Miyamoto, S., & Greenwood, D. (2022). What Individuals Want to Hear at the Point of Type 2 Diabetes Diagnosis. Clinical diabetes : a publication of the American Diabetes Association, 41(1), 110–119. https://doi.org/10.2337/cd21-0151
Polonsky, W. H., Capehorn, M., Belton, A., Down, S., Alzaid, A., Gamerman, V., Nagel, F., Lee, J., & Edelman, S. (2017). Physician-patient communication at diagnosis of type 2 diabetes and its links to patient outcomes: New results from the global IntroDia® study. Diabetes research and clinical practice, 127, 265–274. https://doi.org/10.1016/j.diabres.2017.03.016
Detailed Show Notes and Transcript
[00:00:00] Scott K. Johnson: Welcome to BDI Briefs. This is another exciting installment where we take a brief look at important issues about the emotional side of living with diabetes and working in diabetes. Thanks for joining us today. I’m here with Dr. Bill Polonsky. President of the Behavioral Diabetes Institute and Dr. Susan Guzman, Director of Clinical Education at the Behavioral Diabetes Institute. Both are world-renowned diabetes psychologists and two of my favorite people to talk with.
My name is Scott Johnson. I have lived with diabetes for over 40 years and have been active in the diabetes social media space and industry for a long time.
And with introductions out of the way, Bill, what are we talking about today?
[00:00:53] Dr. Bill Polonsky: Thanks, Scott. I want to bring up a subject that really doesn’t get enough attention. And this has to do with what happens to people with type 2 diabetes when they’re first diagnosed. The day they first discover that they have type 2 diabetes. And often not appreciated is What a very difficult moment this is for folks. There’s often a very strong emotional response and often a very strong negative emotional response. People feel frightened about what this means for my future, about how other people are going to see me. Worries about, just the disappointment and the discouragement that I thought I was doing everything as well as I could, and how could this be? This sense of mortality, is my life going to be shortened? So many strong emotional responses that, if not really ever addressed, really can lead to people not really effectively engaging with their diabetes.
So it can lead to people saying, I’m not going to think about it. And can lead to really bad outcomes over the course of time.
So, as healthcare professionals, we know we have this special moment when we are sitting with someone who’s first learning they have type 2 diabetes. How we talk about that with people can have an enormous impact.
And the reason we’re talking about it today is, as we’ve been going through the recent literature, a series of recent articles really struck me.
Small, Qualitative studies that come from our colleagues. I’m going to tell you the name of the first author here. I’m terrified I’m going to mispronounce it, but I think it’s pronounced Boakye; it’s spelled B O A K Y E. So she and her colleagues have really put forward about these three wonderful articles that have been published over the past few years that really have highlighted, first of all, how very common these really profound and worrisome negative emotional responses to the diagnosis of type 2 diabetes can be (https://pubmed.ncbi.nlm.nih.gov/36714250/).
And also, the importance of them also mentioning how rarely these feelings are ever addressed, ever brought up, ever asked about with their health care providers, and how common it is for people not just to be frightened and worried about the future but feel abandoned with their type 2 diabetes, like not really quite sure what they need to do next, and feeling like there’s anyone really on their side that’s really supporting them.
And she’s also, she and her colleagues have highlighted in these articles what patients want and what they need, how they want to be asked about some of their feelings about learning they have diabetes; they have their questions answered and are offered better support. So, I highly recommend you check out some of these articles. They’re in Clinical Diabetes and Diabetes Spectrum, just published over the past couple of years.
The bottom line is that what these articles have told us brings up something that we’ve actually known for many years: there’s this enormous problem, and we can do better. What should we do, and how do we go about that? Now, I’m proud to say we have looked at this over the years by my colleagues and myself over the past few decades.
In fact, way, way long ago, way back in 2017, we actually published the first of a series of articles where we had surveyed more than 3, 500 people around the world. It was from 26 countries. And we asked them, these were all people with type 2 diabetes, about what happened to them when they were diagnosed, both good and bad, and specifically, we wanted to know what happened to them in their interactions with their health care provider.
And one of the things we focused on is what happened at those moments that was really good for you. That helped you to feel okay about living with type 2 diabetes over the course of the next few years and actually taking on the tasks of type 2 and feeling okay about it and being able to succeed.
In our studies, these two elements really stood out. And when I tell you, you’re going to go, of course, but it’s hard to put into practice often.
One is the degree to which healthcare providers managed to put forward messages to these newly diagnosed patients that were encouraging.
To let people know that this is not a death sentence that you have type 2. Odds are pretty good here in the 21st century. Odds are good you can live a long and healthy life with diabetes with good care and effort. And providing the sense of encouragement about what type 2 means and how you can do. But also doing it, and this is the second point, in a collaborative fashion.
So not just telling people this, but having a conversation. Asking people what their concerns are. Asking them what their questions are. Making sure that people knew that, as best as possible, a person and their health care team are going to do this together. We’re going to meet again soon. We’re going to see where we go next.
We’re going to try to put together a plan that’s doable for you. And those two elements, as it turns out, made an enormous impact on helping people to be successful over time. Now, in these recent articles from Boakye and colleagues–and again, just in case any of her, she, or her colleagues who are listening now, I apologize if I’m saying your name wrong–they’ve really done a nice job in one of the last articles about putting forward these key themes about what we as healthcare providers need to do with our patients. It’s from their 2022 article in their first figure. And this really seems to follow nicely from our own paper. And it’s about the importance of doing this, not just to tell people this, but as a conversation.
So I want to, take a moment and talk about what they’ve put forward in this lovely figure. And I can’t do it as well as my colleague, Dr. Guzman. So Susan, please take us through a little bit of what’s on this table.
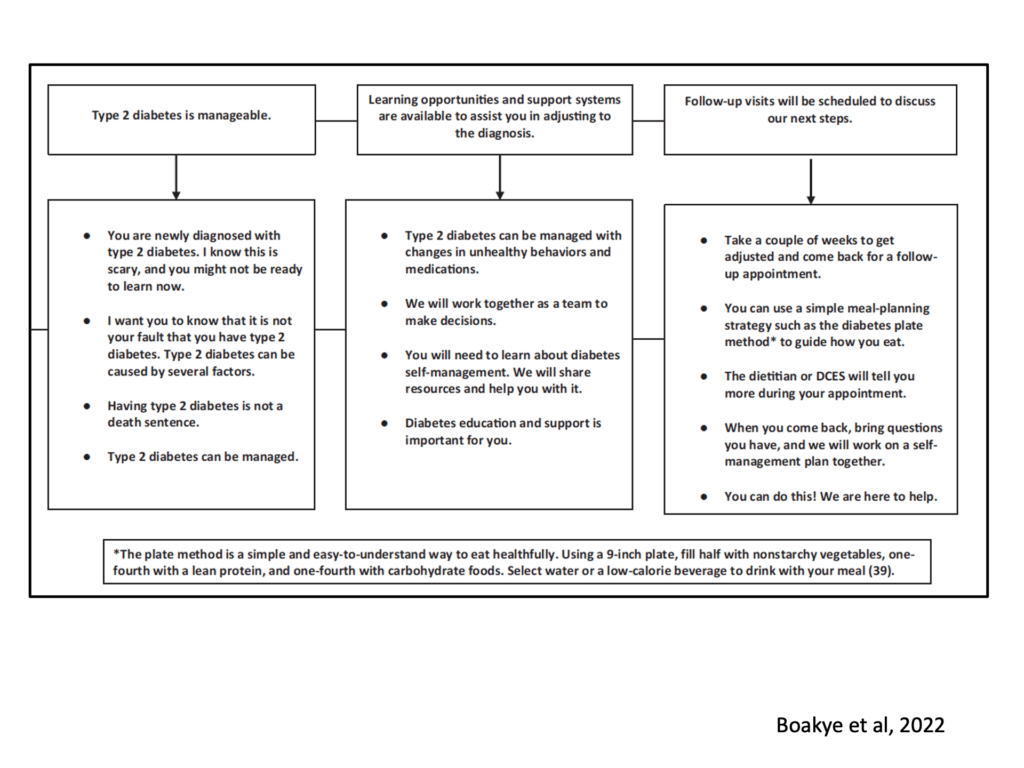
[00:06:49] Dr. Susan Guzman: Yeah, this table actually gives ideas of what you can say as a healthcare professional. The first one is when somebody is diagnosed, you really want to communicate a message of hope, and that de-stigmatizes the experience. And also recognizes there are lots of tough feelings that go with that diagnostic experience of hearing, gee, I, now what? I have diabetes.
So it’s recognizing with empathy that people are hearing bad news. Then, also saying, this is not your fault, and diabetes is manageable. And then following very much, the IntroDia® study that Bill just described, you’re working on a plan for working together with the person that feels doable for them.
And there are some specific ideas of how you can even communicate that. But recognizing that people don’t often want to take action right away. They need a little bit of time to process the information that they now have diabetes and follow up with them in a reasonable time frame to say here are resources that can help you.
That maybe you’re not ready to take action today, but let’s follow up in a couple weeks and then building on that progress over time.
[00:08:05] Dr. Bill Polonsky: Scott, I know you have type 1 diabetes, and we’re here talking about type 2, but like everybody else, you went through some experience of being diagnosed, and you’ve chatted with many people. Through your own blog, who are diagnosed with type one and type two. I’m just wondering how all this strikes you.
Does it make sense? Do you see what’s been missing for folks? What do you think?
[00:08:25] Scott K. Johnson: Yeah, definitely. It definitely makes sense to me. I often think about the experience of someone newly diagnosed with any type of diabetes, really, but take type 2, just for example; they’re often in with a family practice doctor or general practitioner, and they learn they have diabetes and they’re sent out from that appointment and sometime later in that day, they have to face their first meal, now living with diabetes, and I just imagine how terrifying that is to deal with that, not having had any education yet, or really knowing what that means.
I think this makes a lot of sense and really hits home for me.
[00:09:05] Dr. Bill Polonsky: Thank you. What we see, as you just saw and what Susan presented from that lovely article, these elements that we wanna make sure we share with our patients who are newly diagnosed with type two diabetes. I just wanna remind you it’s not a matter of just telling people stuff, but it’s how we make this a conversation, a two-way conversation so that we make sure we’re addressing people’s concerns. And following a similar path, I’m proud to let you know that here at the BDI we put together a booklet many years ago that tried to address many of these particular issues, and it was a booklet specifically for people with type 2 diabetes who were newly diagnosed, because we saw this issue.
And we saw this issue not just with people being concerned and freaked out and not knowing what to do, but sometimes being overwhelmed with information about what to do, that also led them to feel paralyzed and not sure where to go. So this booklet is called the Don’t Freak Out Booklet. And it’s freely available on our website.
Dr. Bill Polonsky: You can print out a PDF or you actually can order copies in there in the booklet form. You can find this on our website, but I want to take you through a little bit of the booklet because, again, I think it’s so representative of what we’re talking about today and how useful it can be. To be fair, it’s just a little booklet, so I like to think of it as not just for someone to look at and read, but in, terms of how this can work in a conversation with one’s health care provider, to look at some of these issues and to talk about them together.
So here’s just a few of the ten tips, ten things we think people need to know when they’re first diagnosed. So just randomly, let’s start with number two, one of my very favorites, which is titled “This Isn’t Your Grandmother’s Diabetes.” And I’m sure this is going to make sense to you. I already said this a little bit earlier.

It’s this idea that if you’ve only known about type 2 diabetes because you’ve seen something terrible happen to someone in your family years ago, that’s then, this is now the 21st century. And again, the message we put forward here at the BDI is so clearly over and over again, with what we call evidence-based hope, is that we know that with good care and effort, odds are pretty good you can live a long life with diabetes, both type 1 and type 2. And that’s what we’re trying to get at with this particular item. So that’s number two. Number three, is called Diabetes is Not Your Fault. Susan, you do this better than me. Tell us a little bit about why this issue is so important.
[00:11:41] Dr. Susan Guzman: Now we know this. The stigma around diabetes is pervasive and profound, and feeling blamed when you have diabetes, both when you get it and for people who aren’t reaching treatment targets, really feel shamed, blamed, and judged. And this is really getting at pushing back on the idea that diabetes is not your fault.
Nobody chooses to have diabetes. And really rethinking it as something that you now have and there’s a lot that you can do to manage. So push back on shame and blame and also accept now that you have it there’s a lot you can do.
[00:12:17] Dr. Bill Polonsky: Thanks, Susan. And let’s just mention one more of the ten items here. That’s actually another one of my favorites, which is number six. And I think I just like the picture more than Any of the other pictures we have in our booklet. But it really gets at another issue that often times people will say and worry about when they’re first diagnosed, which is, how is my eating going to be restricted?
Dr. Bill Polonsky: And so you can see the title here. No, you won’t be limited to eating nuts, twigs, and birdseed for the rest of your life. That we know things are doable. We know that here in the 21st century, we have ways to make it possible and easy for one to eat in moderation, to eat the things that you really love.
Changes are likely to be needed if you want to be successful. But you won’t have to live in a state of deprivation. It’s just not true. In fact, we know a diabetes-friendly way of eating is a healthy way of eating, really, for all of us. So, I encourage you to check out our 10 Things booklet, if you’re a health care provider, think about how you can use that in conversation with your patients, especially when they’re newly diagnosed, because, again, we see this as such an important moment that doesn’t get enough attention.
Again, let’s all do our best, both person with type 2 diabetes and health care provider, to think harder. Think harder about how we can make this better for that moment when you first learn you have type 2 diabetes, even if you’re a busy health care provider and time is limited. We can do better. It’s an important moment.
What happens in that moment can reverberate over the course of years. I encourage all of you to consider it. Think about it. Let’s all get more creative. Thanks for listening. Scott, take us home.
[00:14:02] Scott K. Johnson: Alright, big thanks to everyone watching, and thank you two for just shining some light on these important moments in the experience of living with diabetes and helping us all see that we can live well with diabetes.