Introduction
Welcome back to another installment of BDI Briefs! Today we’re diving into an important topic: assessing diabetes distress. I had the pleasure of speaking with two experts and pioneers in the space, Dr. Bill Polonsky and Dr. Susan Guzman from the Behavioral Diabetes Institute. They shared their insights on the history of assessing diabetes distress and what methods may be best today.
The Evolution of Assessment Tools
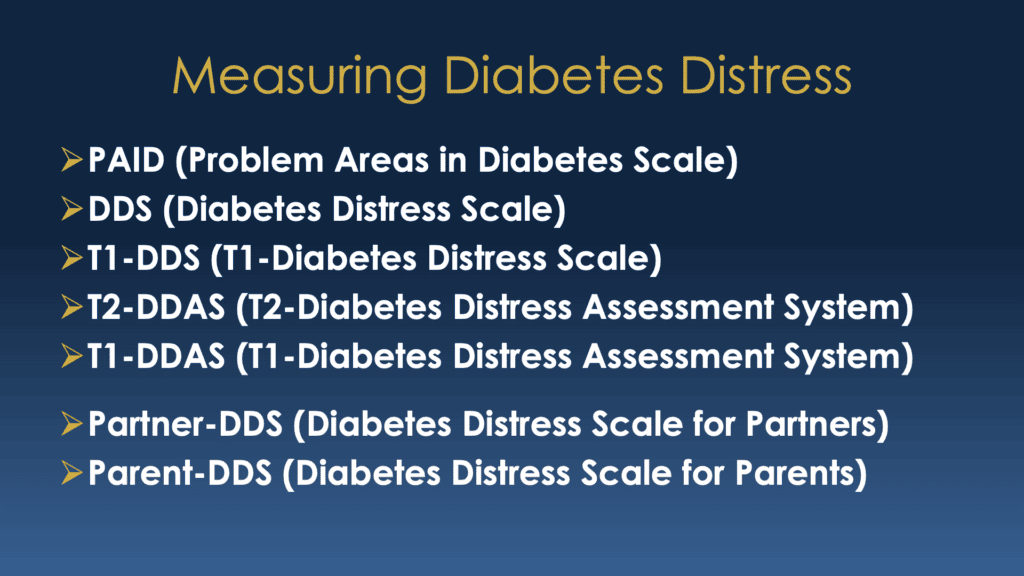
Over the past 30 years, numerous tools have been developed to assess diabetes distress. Dr. Polonsky described the various assessment tools that have been developed over the past 30 years. He feels this abundance of tools can sometimes confuse clinicians about which one to use. Here’s a quick rundown of the main tools discussed:
- PAID (Problem Areas in Diabetes Scale) – Developed in 1995, this 20-item questionnaire is one of the most widely used tools globally.
- DDS (Diabetes Distress Scale) – A shorter, 17-item tool developed 10 years after PAID, with four subscales to drill down into specific areas of distress.
- T1-DDS (Type 1 Diabetes Distress Scale) – A 28-item tool focusing more specifically on issues faced by people with type 1 diabetes.
- T1-DDAS (Type 1 Diabetes Distress Assessment System) – The latest tool with an 8-item core scale and ten short subscales, addressing modern concerns like technology distress.
- T2-DDAS (Type 2 Diabetes Distress Assessment System) – Similar to the T1-DDAS but tailored for type 2 diabetes, with seven source scales.
Why So Many Tools?
The evolution of these tools reflects the growing understanding of diabetes distress. Dr. Guzman emphasized that the latest tools, like the T1-DDAS and T2-DDAS, are designed to capture 21st-century concerns that older tools might miss because those concerns didn’t exist at the time. Like some of the diabetes technology many of us use today, for example. You wouldn’t have been distressed by CGM alarms back in 1995 because they didn’t exist yet.
Dr. Polonsky feels he and his colleagues may have made a mess of the situation by creating so many different assessments. But it feels like a very natural path of growth and learning to me. Of course, tools and approaches change as experts dig in and learn more.
And I would rather have the tools be available, even if messy, than not exist at all.
Practical Advice for Clinicians
The recommended method for assessing diabetes distress depends a lot on the group of people with diabetes. Dr. Polonsky walks through each of these in more detail, and in general, the newer methods are recommended where possible.
For clinicians juggling mixed samples of patients with type 1 and type 2 diabetes, Dr. Polonsky recommended using the 8-item core scale from the T1-DDAS and T2-DDAS. It’s short, comprehensive, applicable to both groups and a great way to determine whether you need to dig deeper.
He also advised against relying solely on an older, two-item screener, which may miss critical aspects of diabetes distress. All of the tools, except for PAID, are available on the Behavioral Diabetes Website.
Empowering People with Diabetes
One of the most exciting resources discussed was DiabetesDistress.org. This site allows individuals with diabetes to complete these scales, get immediate feedback, and save their results as PDFs to discuss with their healthcare providers.
It is completely free and none of the information is saved or stored. It’s a great way to identify specific areas of distress and start a meaningful conversation about how to address them.
Final Thoughts
I’m incredibly grateful for Dr. Polonsky, Dr. Guzman, and their colleagues’ work. Their efforts to understand and address the emotional side of diabetes make a huge difference in our lives.
While the landscape of diabetes distress tools might seem messy, it’s a testament to their progress in recognizing and addressing these crucial issues.
If you’re feeling overwhelmed by your diabetes management, know that you’re not alone. There are tools and people ready to help. Check out the resources available, talk to your healthcare provider, and take proactive steps to manage your emotional health.
Detailed Show Notes and Transcript
[00:00:07] Scott K. Johnson: Welcome to BDI Briefs. This is another exciting installment where we take a brief look at important issues about the emotional side of diabetes. Thanks for joining us today.
[00:00:18] Scott K. Johnson: I’m here with Dr. Bill Polonsky, President of the Behavioral Diabetes Institute, and Dr. Susan Guzman, Director of Clinical Education at the Behavioral Diabetes Institute. are world-renowned diabetes psychologists and two of my favorite people to talk with. My name is Scott Johnson. I have lived with diabetes for over 44 years and have been active in the diabetes social media space and industry for a long time.
[00:00:46] Scott K. Johnson: And with introductions out of the way, Bill, what are we talking about today?
[00:00:50] Dr. Bill Polonsky: Scott, thanks. we want to talk about something that I think is important to mostly clinicians, but actually for some people with diabetes as well. We have talked a lot about this whole idea of diabetes distress, why it’s so important to folks with diabetes, and how we expect and hope that clinicians will pay attention to this when they’re working with their patients.
[00:01:12] Dr. Bill Polonsky: Susan is involved in a huge program with our colleague Larry Fisher, training staff all over the country about how to use this concept of, the widespread problem of diabetes distress, but we don’t talk enough about how actually you should assess it. And to be honest, we wanted to use this time almost as an apology, because it’s people like me and my colleagues that have made a real mess.
[00:01:41] Dr. Bill Polonsky: And when I say a mess there’s a lot of ways to actually assess diabetes distress, and that means using self report questionnaires, typically, that people can use on their own, or their clinicians could use, as a way to, as conversation starters, to say, what’s really going on with this person? How really can I be of help?
[00:02:02] Dr. Bill Polonsky: We have developed so many different measures of how to assess this issue. Over the past 30 years, what we’re seeing is clinicians all over the world are going, which one am I supposed to use? So we wanted to just give you a little bit of lay of the land, and hopefully this will be helpful. first of all, here’s what we’ve done.
[00:02:25] Dr. Bill Polonsky: Over these 30 years, we’ve developed 7 different ways of assessing diabetes distress. And you can see that on this screen. The first one we developed way back in 1995 is called the PAID, the Problem Areas in Diabetes Scale. And we’ll talk a little more about all these in more detail in a moment. Then 10 years later, we developed what we thought was a better version.
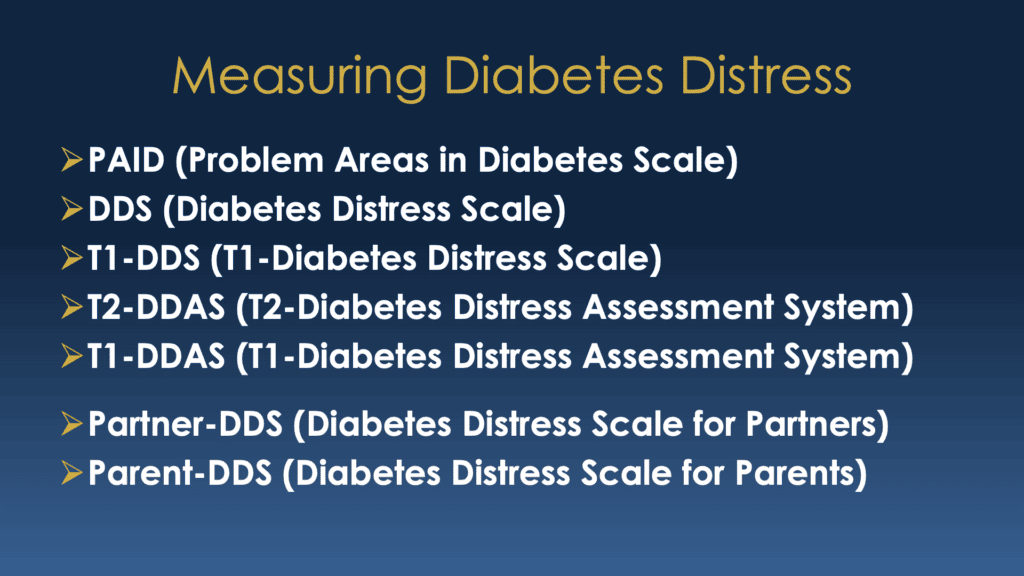
[00:02:46] Dr. Bill Polonsky: We called it the Diabetes Distress Scale. Then actually 10 years after that, we said, we should really get a little more focused on who these instruments are for. We developed the T1 or Type 1 Diabetes Distress Scale. And just in the past couple years, we’ve gotten even fancier. And we have what we actually think are now the best instruments, both the Type 2 Diabetes Distress Assessment System and the same thing for Type 1s, the T1-DDAS.
[00:03:12] Dr. Bill Polonsky: And by the way, there’s more, as you’ll see on the bottom of this slide. We actually have diabetes stress scales for partners, especially for those who have, partners of people with type 1 diabetes, and a scale for parents who have, especially teenagers who have type 1 diabetes, special groups we’ve been most concerned about.
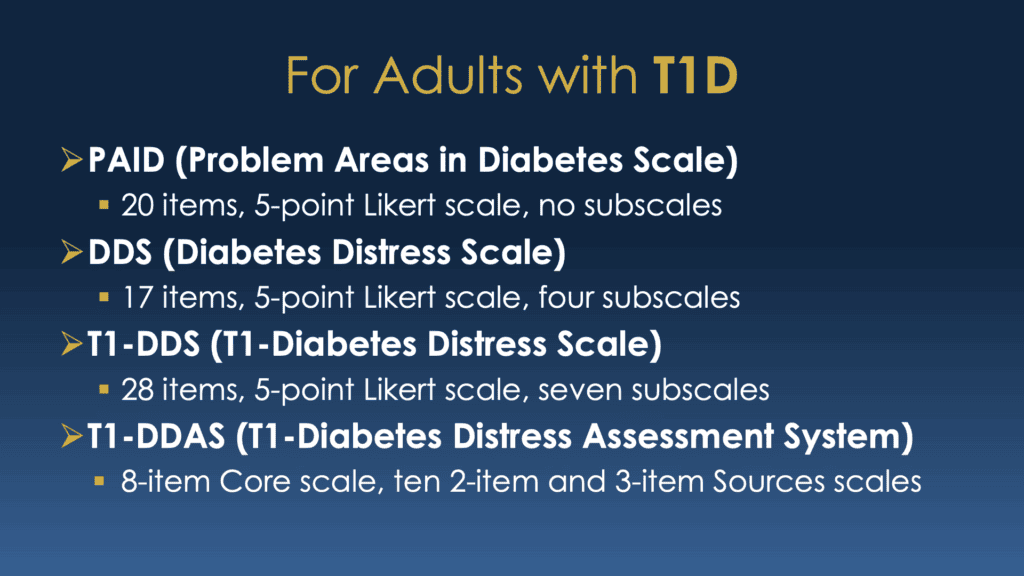
[00:03:30] Dr. Bill Polonsky: We’re not going to talk about those last two, because we’d be here all day, it’s so complicated. But we just want to talk about these five, and what do we recommend about what’s the best thing to use now in the year 2024? So first of all, we could easily divide this up and say if you are a person with type 1 diabetes, or you are a clinician, and you want to really understand better what’s going on with your patients.
[00:03:56] Dr. Bill Polonsky: So on this next slide, you’ll see here are the instrument options that you have, and there’s four of the five we just mentioned. And we’ll talk a little bit more about these in some detail. Susan’s had a lot of experience with all of these, so maybe more than I have at this point, so I’m hoping she’ll be chiming in shortly as well.
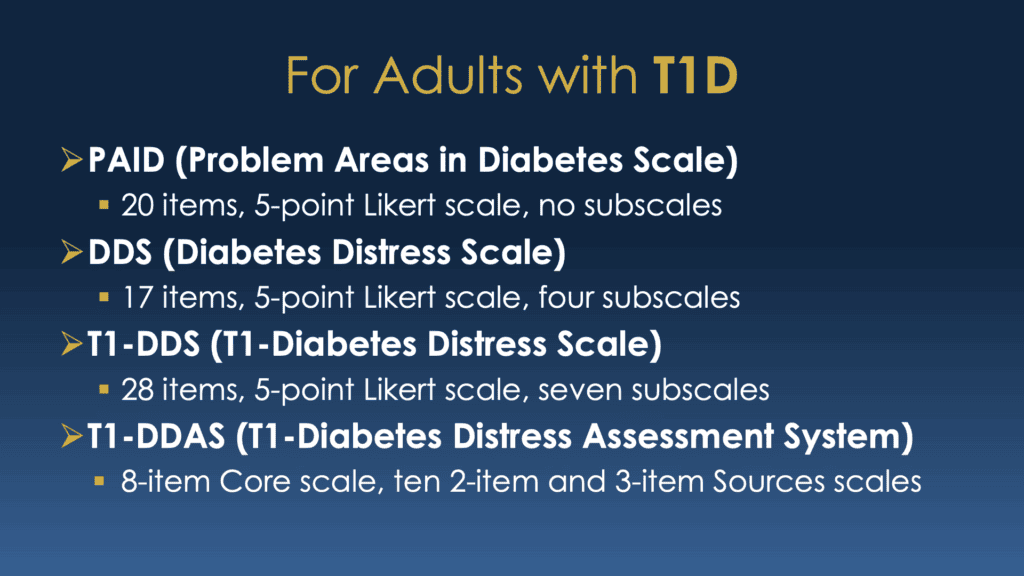
[00:04:16] Dr. Bill Polonsky: Again, you can always go back to the PAID, although it was originally developed for people of type 1 and type 2, we didn’t specify for people of type 1. It’s probably still the most popularly used measure around the world, despite my best efforts to try to convince my colleagues that it could improve since then.
[00:04:33] Dr. Bill Polonsky: But the PAID is still widely used, it’s 20 items. The other choice is the Diabetes Distress Scale, the DDS. Again, this is, It was developed for people with type 1 and type 2. It’s a little shorter, with 17 items, and it has these four subscales that allow us to drill down a little bit about what’s really going on with this individual.
[00:04:54] Dr. Bill Polonsky: Another option, about 10 years after that, was the type 1 diabetes distress scale. Now it’s a little longer, it’s 28 items, but it has a bunch more subscales and really focuses on the issues for people with type 1 much better. But we couldn’t leave it alone, so just very recently, my colleagues and I, in this case led by, my friend, Professor Larry Fisher, published the Type 1 Diabetes Distress Assessment Scale.
[00:05:23] Dr. Bill Polonsky: I know, it’s already a mess, assessment system, I should say, which has this eight-item core scale which really gets at the heart of what the emotional core of diabetes distress, and then these ten very short subscales. To help us understand what the sources are, what’s going on, what’s contributing to why this person’s going outof their their minds about this. So if you’re worried about assessing type, distress and type one, you could use any of these.
[00:05:49] Dr. Bill Polonsky: But as far as we’re concerned, we think each of our skills has gotten better over time. And so I would say the best is the last one, T1-DDAS not,
[00:06:00] Dr. Susan Guzman: I’d like to add just quickly, Bill, that one of the nice things from the T1-DDAS, the newest one, is that it does have some, a source scale that looks at technology distress, which is something the others do not. And also, more around health care instead of just, looking at a physician, as in the previous, Type 1 Diabetes Distress Scale.
[00:06:25] Dr. Susan Guzman: So it, we listened to people when they said, this misses this or that. there’s, new source items that are in the latest T1-DDAS that the others miss.
[00:06:38] Dr. Bill Polonsky: thank you for making that point. And that’s exactly why we recommend that this latter scale, the T1-DDAS more than the others. Because, for that scale, we really looked at what’s changed, what’s important to people with diabetes. What are the new things driving people crazy that are true now, 2024, which didn’t really exist or people weren’t talking about back when we first, developed and published the PAID in 1995.
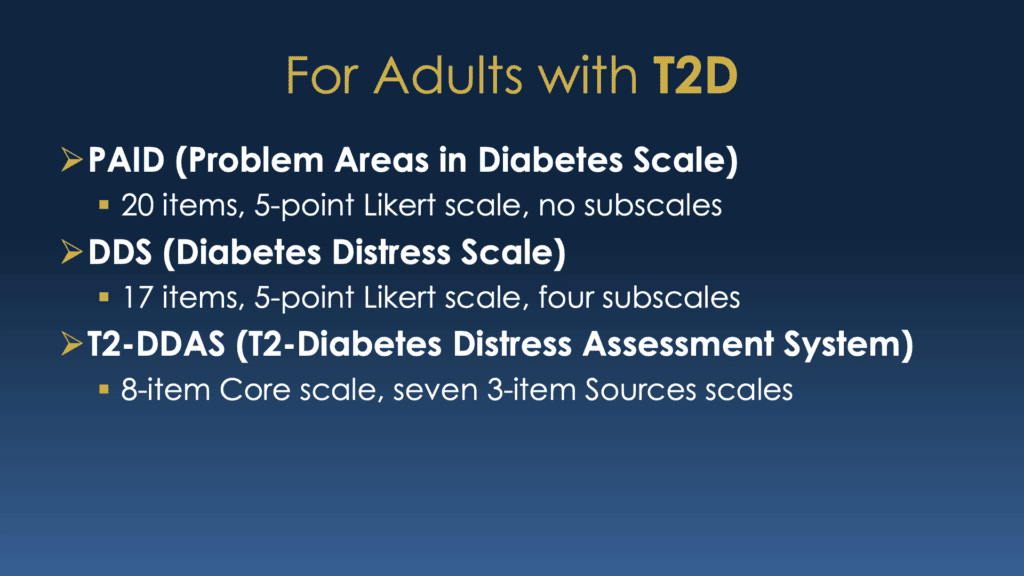
[00:07:04] Dr. Bill Polonsky: So things have moved along. We’re trying to move along with it, and that’s why we think this last scale is probably your best option. So let’s type 1 let’s look at the next slide, which is really about the scales for type 2. So here the choices are three. I’ve already mentioned the first two. Again, the PAID, which could be used for type 1 or type 2, the Diabetes Distress Scale.
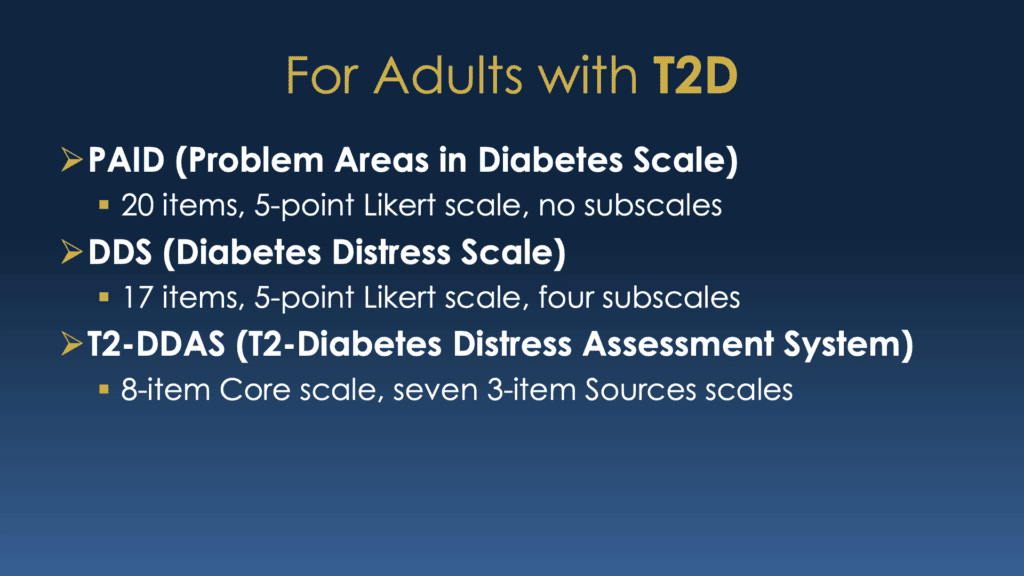
[00:07:28] Dr. Bill Polonsky: Again, it’s a little better, but again, it’s still for either group. And then finally, just like we talked about with the type 1 scale, we have a new contemporary scale for people with type 2 diabetes. In this a, this part of the 21st century, so the T2-DDAS, the Diabetes Distress Assessment System, again, more contemporary and up to date, and perhaps most importantly, it has that identical eight item core scale that really gets at the emotional aspect of diabetes distress.
[00:08:04] Dr. Bill Polonsky: It has now, not 10 but seven source scales to help us zero in on these 21st century concerns for people, and that’s why. If you had, if I had to pick, I’d say the T2-DDAS is the best choice for folks with type two. again, I want to remind you that eight item core scale is the exact same core scale that we have for in the T1-DDAS.
[00:08:28] Dr. Bill Polonsky: And that’s gonna be important, as we’ll see in a moment on the next slide. But let me stop for a moment, say, Susan, any thoughts about this?
[00:08:35] Dr. Susan Guzman: You covered it. And the eight-item core scale, I think, is key.
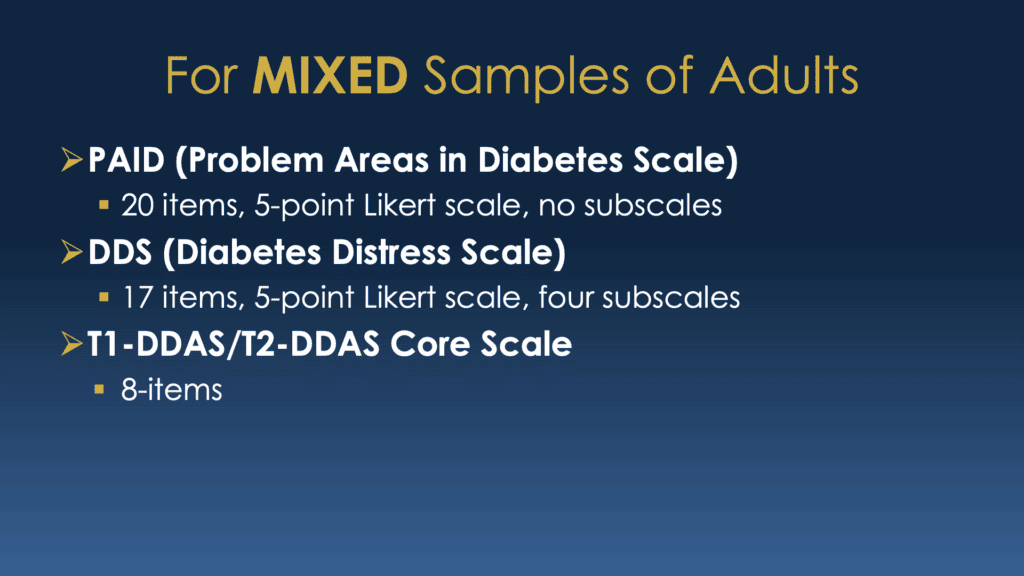
[00:08:41] Dr. Bill Polonsky: So one more issue that comes up, and certainly it’s gonna be true for those of busy clinicians or researchers, is you’re gonna say, I got. I want to use one scale, and I’ve got a mixed sample. I’ve got people with type 1, I’ve got people with type 2, who knows? I want something that’s going to work for everybody.
[00:08:57] Dr. Bill Polonsky: So again, just to be repetitive. You can still use the PAID just like it’s been used all this time. You can still use the DDS, the Diabetes Distress Scale. What we think is a better choice is this 8 item core scale. The core scale that was developed for the T1-DDAS and the T2-DDAS. One of the things we like about it so much, it’s really short.
[00:09:22] Dr. Bill Polonsky: Eight items. That’s it. now you could use more, but if it’s a mixed sample, just those eight items, and that’s what we see more and more busy researchers are doing. They simply don’t want to overwhelm people with too many items. And that eight item core scale is very valuable. And by the way, we know that some of you have used something, I hate to say this, something else we developed years ago, which was a two item screener, a diabetes distress screener.
[00:09:50] Dr. Bill Polonsky: And if I remember correctly, these were items that came from the DDS, the Diabetes Distress Scale and we have seen that two item screener being used in studies and in practices all over the place. We just don’t think it’s a very good idea. People are using those, that two item scale, hard for me to call it a scale, and thinking that’s measuring diabetes distress.
[00:10:14] Dr. Bill Polonsky: But it’s really, it’s just a screener. So if you want to keep things really short because you’re doing a research study or you’re worried about overwhelming your patients, just use that core scale – the last thing on this slide that you have right in front of you.. Susan, I think you support that idea a lot.
[00:10:32] Dr. Bill Polonsky: Any thoughts about that?
[00:10:35] Dr. Susan Guzman: Yeah, I think that we’re gonna miss a lot of folks if you’re only using the two items. as a way to indicate whether a person has distress or not. and really we would like to argue that, use the whole subscale. We know that’s not realistic in a lot of settings or, perhaps in research, but we know that, people may have one source scale that’s elevated and that’s worthy of a conversation.
[00:11:04] Dr. Susan Guzman: And if you think about not thinking of measuring distress as like a, as a, indicating a pathology or a mental health disorder, but rather somebody’s saying, in regards to the emotional side of diabetes, I’m having challenges. And these challenges are worthy of a conversation. And so in terms of a clinical conversation, we think that we’d like people to be assessed in a more comprehensive way.
[00:11:31] Dr. Bill Polonsky: Yeah that’s perfect. Now to be fair, if you think about that first slide I showed you, where we had these all seven scales, and I said we’re going to focus on these first five. There’s other good reasons why people are still going to go back and use the PAID or the DDS or the T1 DDS and it comes, it has to do with other things.
[00:11:51] Dr. Bill Polonsky: Maybe you want to use this scale in a study that’s in a different language. for these, our new scales, the T1 and T2 DDAS, they’re new. We don’t have them in a lot of other languages. Spanish, maybe one more. But the DDS, for example, which has now been used for 20 years, is available in almost 40 languages.
[00:12:12] Dr. Bill Polonsky: And all of these you can find on our website at behavioraldiabetes. org. And they’re, all of this, except for the PAID I should say, all of these are freely available to people with diabetes, to researchers, to use anywhere, any way they want. So feel free to check it out on our website, behavioraldiabetes.org.
[00:12:33] Dr. Bill Polonsky: We don’t have the PAID on our website. We don’t, that’s the one, instrument that we don’t hold the copyright to. If you’re interested in doing research with the PAID you should contact the copyright holder, which is my old employer, the Joslin Diabetes Center in Boston. Now, the other thing I want to mention, a thing that I think we’re really proud of, if you’re interested in not going to our website and downloading these instruments and taking a look at them, but wanting to try them, now, there’s this other really interesting thing you should know about that I think we talked about briefly before, and I’m going to show you one more slide so you can see what that page looks like.
[00:13:11] Dr. Bill Polonsky: And it’s called, DiabetesDistress.org. And what we’re so proud about DiabetesDistress. org, is of those first five scales, except for the PAID all other four are freely available for you to check out and use and get feedback for right here, right now. You can go to this scale, you can go to this website, you can complete the scale just by touching the right, whatever numbers make sense to you as you fill it out, feel free to check it out any time you want, and it’s automatically scored, and it gives you a little summary page so you can see how you scored in terms of, the total score, what the sub scales are, the source scales, the core scale, whatever, whichever instruments you might pick. We have them all in English and Spanish on this website.
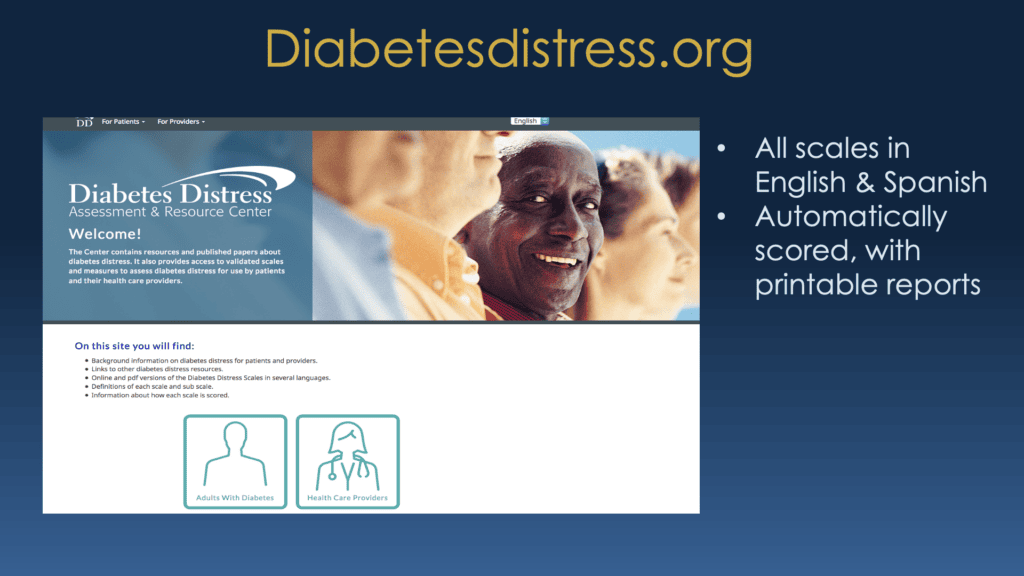
[00:14:02] Dr. Bill Polonsky: And, there’s a little bit of information, not as much as we’d like about what to do about it, but again, it’s designed to just promote thinking, to open a conversation, and to really begin to have a better way of looking at what’s driving you crazy about diabetes and what do about it. We invite you and encourage you to check out the website, DiabetesDistress.org
[00:14:22] Dr. Bill Polonsky: or if you’re interested in downloading copies of any of these instruments in whatever languages you might need them in, you can find them on our website, BehavioralDiabetes.org. I don’t know, that’s about all I’ve got. Susan, Scott, what do you think about any of this? Any thoughts, comments?
[00:14:39] Scott K. Johnson: I’m just so excited that these tools exist, and I actually, I smile to myself hearing you say that, boy, we’ve made such a mess of this, because I would rather have it be messy and available than how it looked 40 years ago when no one was thinking about the emotional health and emotional well-being side of living with diabetes.
[00:15:00] Scott K. Johnson: it also makes perfect sense to me that the more that you in the field explore and learn and discover, that everything around it evolves. I’m just so thankful for people like you and the work you’re doing. It makes my life a lot better. So thank you.
[00:15:17] Dr. Bill Polonsky: Thanks Scott. Susan, anything else? Any thoughts about this?
[00:15:23] Dr. Susan Guzman: I just would like to add that if you’re a person with diabetes, you can go on the diabetesdistress.org and take the appropriate distress measure for your type of diabetes and it automatically scores and you can save it as a PDF and show it to your healthcare professional if there’s something or make an appointment with a diabetes care and education specialist.
[00:15:47] Dr. Susan Guzman: If you don’t know what to do about it, cause that’s sometimes we get notes like, duh, I have distress around my diabetes. Now what? it’s an opportunity then to take action and that’s how we would like to think about it. You may know already that you, if you have distress, that you’re distressed, but it gives you an opportunity to see what particular areas and have a name for what is bothering you and be able to then focus and have a conversation with maybe action steps that you can take to feel better.
[00:16:19] Dr. Bill Polonsky: I hope someday, we’ll get enough, good funding to be able to actually add to this website, to really give people even more comprehensive feedback about what their fingerprint, their diabetes distress fingerprint really looks like and how high they score on different scales and subscales and source scales and what that means and what we’ve learned about where that goes.
[00:16:38] Dr. Bill Polonsky: So it’s not as populated as we would like, but I do hope it’s a good start for folks. Following up, one last thing that Susan mentioned, if you do use the diabetesstress.org site, do feel free to play, because none of this gets saved unless you, as Susan said, unless you want to save it as a PDF. So all this is completely anonymous.
[00:16:57] Dr. Bill Polonsky: We’re not scoring or saving anything. know that this is available for you for your use and for clinicians. Again, feel free to use this in any way that makes sense for you. As long as it’s supporting your efforts to help your patients, to be successful in managing their diabetes and feeling better every day, as I think Scott said so elegantly.
[00:17:18] Dr. Bill Polonsky: So that’s really all I think we’ve got to say. So Scott, please take us home.
[00:17:23] Scott K. Johnson: All right. It’s my pleasure. Again, thank you to both you, Dr. Guzman, Dr. Polonsky, and all of the people you’ve worked with to help make this happen and everyone else working on the emotional health side of living with diabetes. I’m very grateful. Big thanks to everyone watching. It’s just refreshing to talk about these things in a positive light and hopeful action step-type messages.
[00:17:50] Scott K. Johnson: It makes a big difference. That is what we like to do here, and we are excited to do more of that in our next episode. We hope to see you then. Thanks.

