Continuous glucose monitoring is an important part of my diabetes management. I don’t like that people covered by Medicare are being denied coverage for this useful tool.
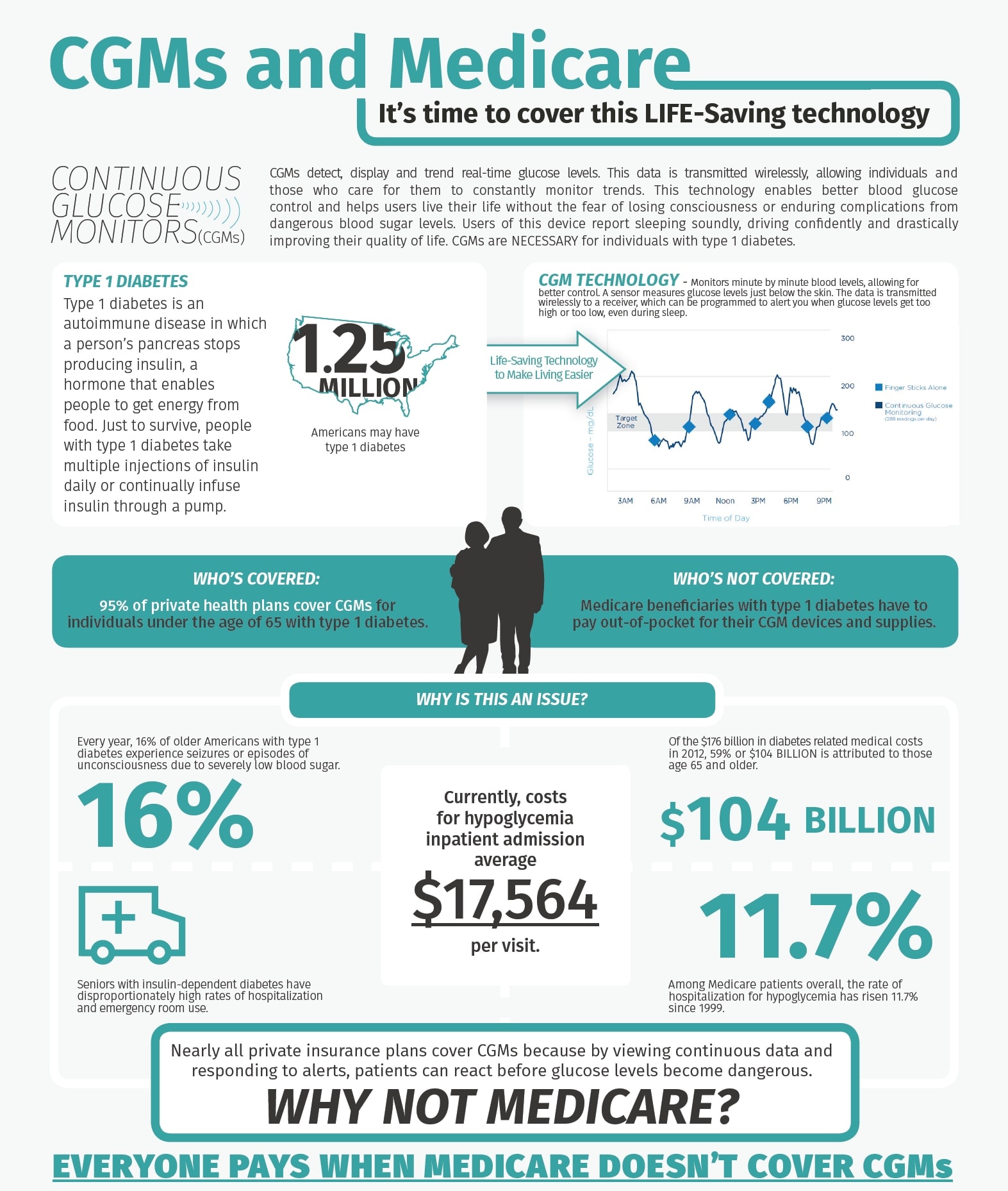
At first blush, it may seem expensive for Medicare to cover CGM’s for their members.
But if CGMs reduce hospitalizations from lows it may actually save money.
How do we change this? DPAC!
Thankfully, we have friends who are passionate about making advocacy simple. Christel & Bennet have worked very hard to build the Diabetes Patient Advocacy Coalition, and through DPAC it is dead simple to send a quick message asking your representatives to support this. You don’t even need to know who they are (DPAC does it for you).
DPAC’s tools are even smart enough to know whether your representatives have already signed on, and if so, you’ll be sending a thank you letter – automatically.
And yes, you can help if you don’t have diabetes. If someone you care about lives with diabetes, let your representatives know that you want their support on this. We need your help too!
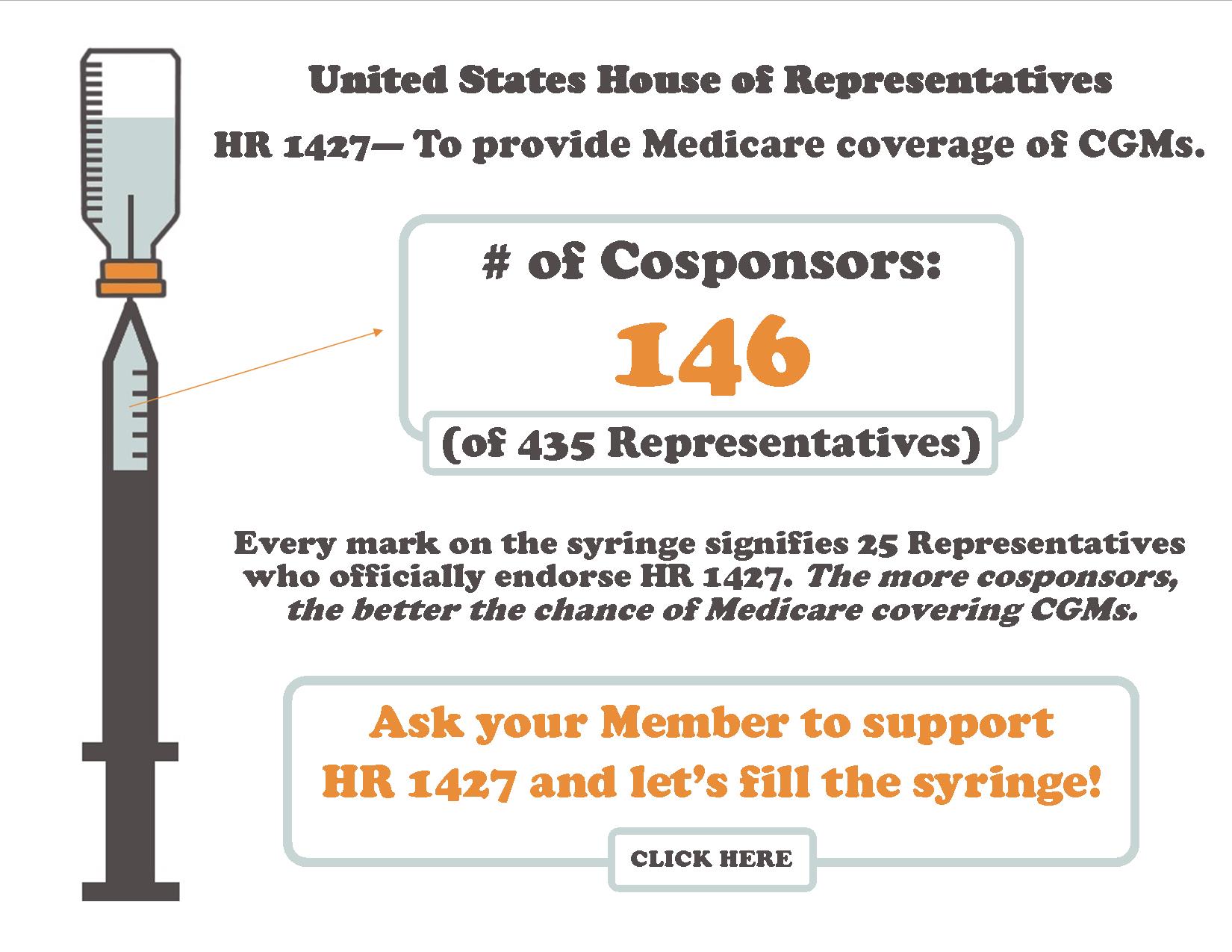
Through DPAC’s easy tools, you can help fill the syringe…
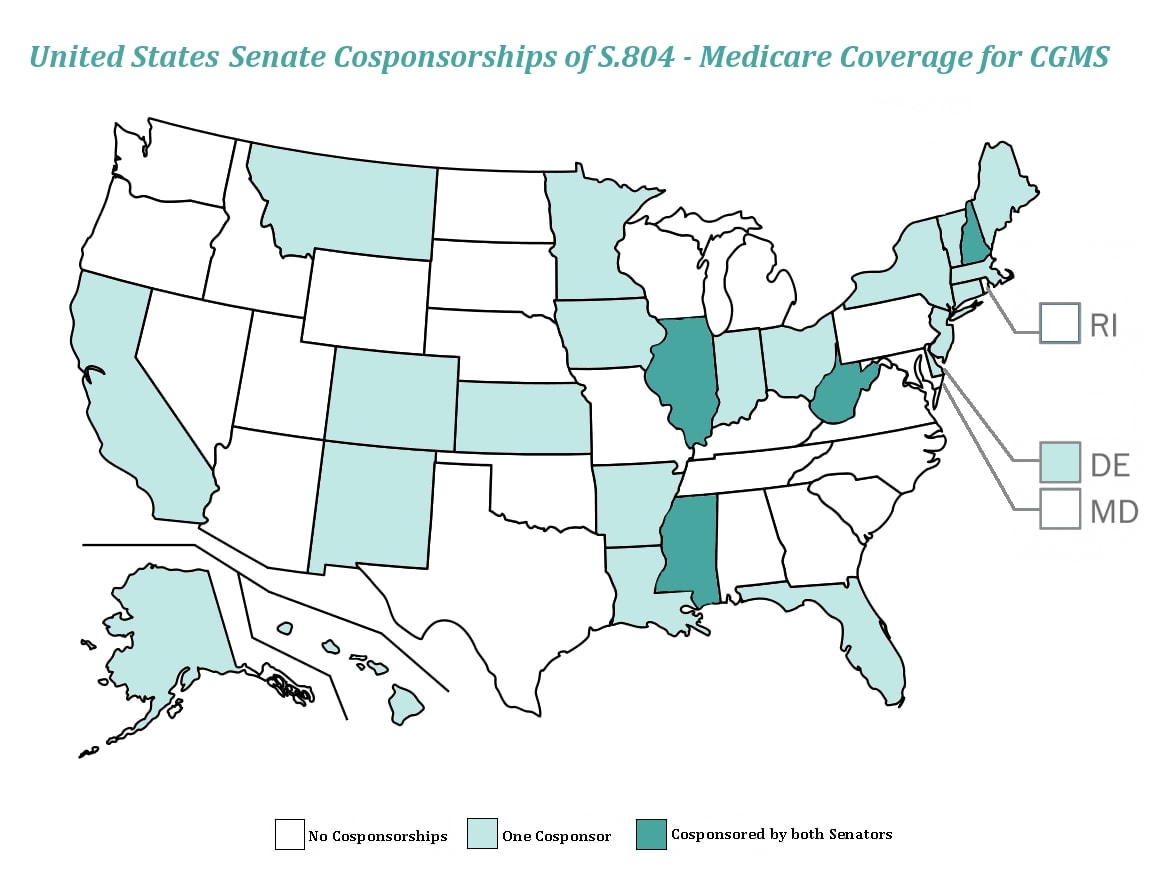
And help color the map…
Please click through to DPAC’s “Send a Message” page. It’s fast, it’s easy, and it makes a difference.
Graphics provided by HCM Strategists. Full-size copies: Medicare-CGM Infographic, House-CGM, Support Map