Welcome to another episode of BDI Briefs! Our aim with BDI Briefs is to take a brief look at important issues about the emotional side of diabetes.
In this short discussion, Scott, Bill, and Susan have a thought-provoking discussion exploring a groundbreaking study titled “Is insulin right for me?”, which delves into the challenges of encouraging people with type two diabetes to consider insulin as a treatment option. The study involved a web-based intervention, and the results were surprising in ways that challenge conventional thinking.
Holmes-Truscott, E., Holloway, E. E., Husin, H. M., Furler, J., Hagger, V., Skinner, T. C., & Speight, J. (2022). ‘Is insulin right for me?’: Feasibility of a pilot randomised controlled trial and acceptability of a web-based intervention to reduce psychological barriers to insulin therapy among adults with type 2 diabetes. Diabetic medicine : a journal of the British Diabetic Association, 39(3), e14759. https://doi.org/10.1111/dme.14759
Detailed show notes and transcript
Scott K. Johnson
Welcome to BDI Briefs. This is another exciting installment where we take a brief look at important issues about the emotional side of diabetes. Thanks for joining us today. I’m here with Dr. Bill Polonsky, President of the Behavioral Diabetes Institute, and Dr. Susan Guzman, Director of Clinical Education at the Behavioral Diabetes Institute. Both are prolific researchers and clinicians in diabetes psychology who do so much for all of us living with and working in diabetes.
My name is Scott Johnson. I have lived with diabetes for over 40 years and have been active in the diabetes social media space and industry for a long time. And with introductions out of the way, Bill, what are we talking about today?
Dr. Bill Polonsky
Thanks, Scott. So glad you’re here and I’m so glad Susan’s here. So we’re going to do something a little different today. There’s some important issues I want to address and to get to those issues, I want to talk about this new study that was just published that really highlights something very important that we deal with quite a bit at the BDI.
This is from our colleagues in Australia. The first author is Elizabeth Holmes-Truscott and her colleagues, and as you can see, the title is, “Is insulin right for me?” It’s a web-based intervention. This is a very unusual publication. It was extremely well done, published in one of our better journals, and it came to some really –well, the kind of conclusions you don’t typically see because this is one of the few studies I have seen published in quite a while where the results were negative, but negative means something really good that we’ll explain.
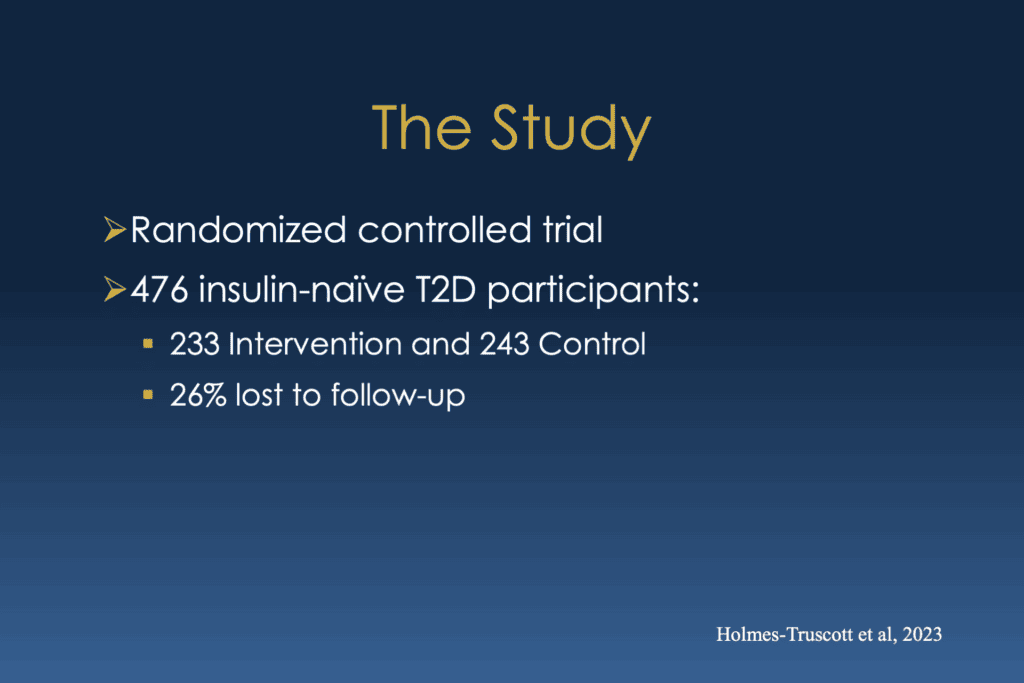
So, to tell you a little bit about this study, again, it was what we call a randomized controlled trial, which is by far the kind of approach, the gold standard that tells us that we can trust the results. They identified almost 500 people in Australia, all of whom had type two diabetes, were not on insulin, and had never taken insulin.
Dr. Bill Polonsky
They randomly assigned about half of them to a “intervention arm”, and the other half to a control arm. Then, they had them go through this intervention, which I’ll describe in a minute. And then decided to evaluate how they were doing about a couple of weeks later and then a few months after that. And they quickly lost about one-quarter of the population, which was just part of the problem they ran into, which is part of our interesting story.
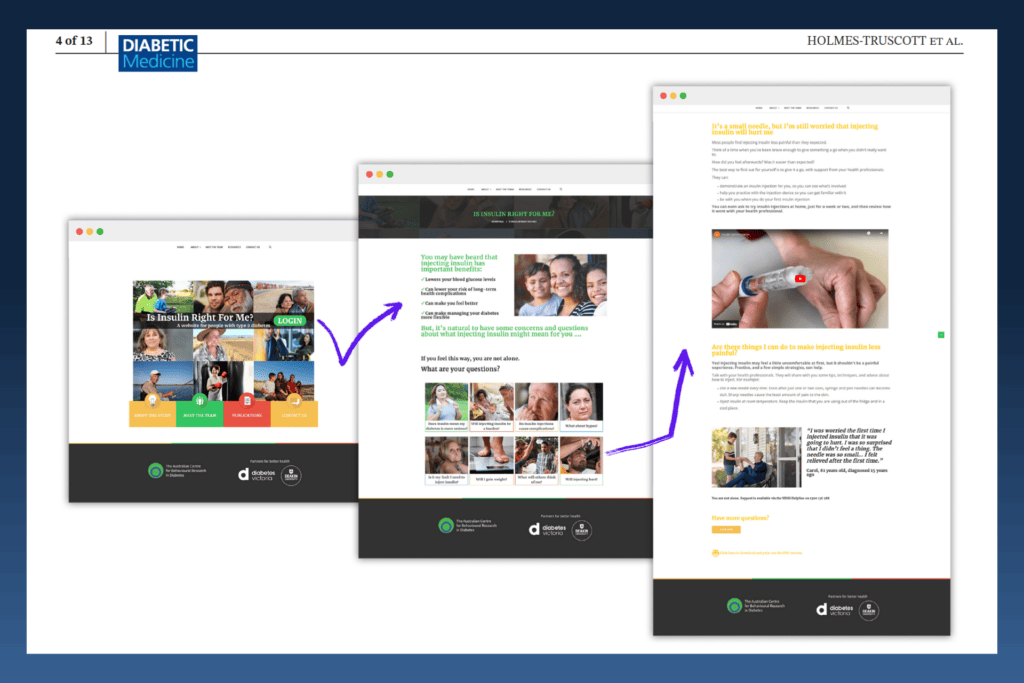
So the intervention was this cool website – I’m so jealous that they had this, and again, this website is, I believe, the title is “Is insulin right for you?” And it’s this fascinating multimedia site where someone could go on and learn about the positives and negatives of taking insulin and really focuses on evaluating “Well, what are you concerned about?”, “What do you think are the obstacles?” And “If you ought to worry about taking insulin.”
They focused on eight particular barriers and, using all sorts of different approaches, looked at encouraging people to think about little differently, seeing what an injection was really like, etc., etc., etc.. It’s really nice website. So they invited this intervention group in the study to please some time over the next couple of weeks, go to this website and check it out.
Dr. Bill Polonsky
There were no formal directions. You know, “You may want to look at one of the obstacles or barriers to insulin, you might want to look at all of them, but take a look and see what’s of interest to you.” Then, they evaluated whether it made a difference after this two-week period and then months later. Now, the control group you just asked to visit another website with boring information about “Here’s everything you need to know about insulin.”
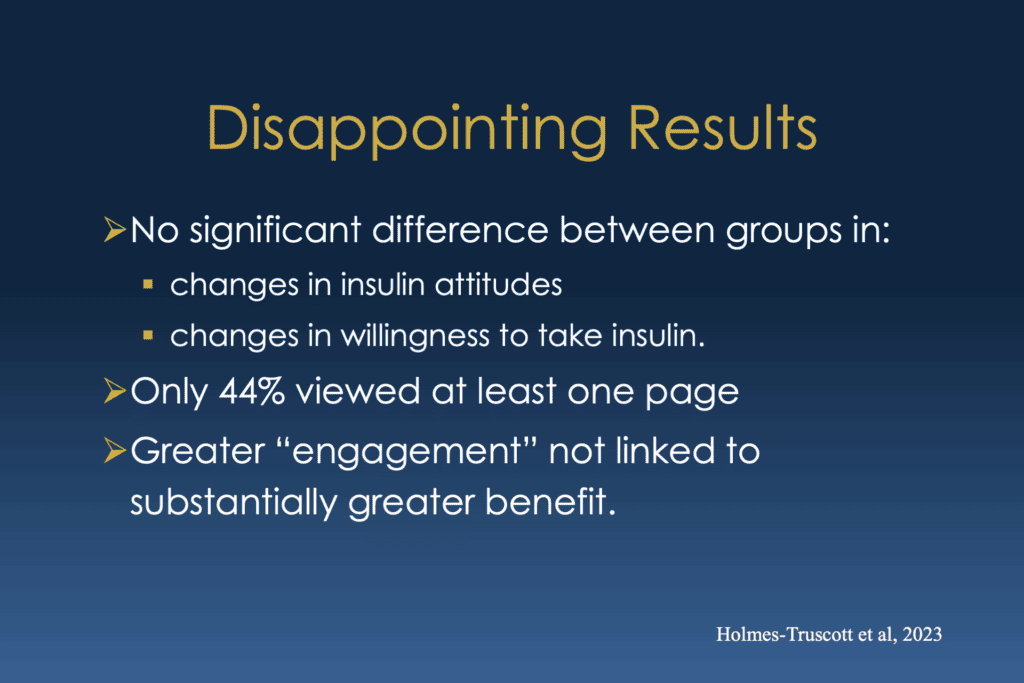
What they found was, well, it was disappointing. You know, it turns out there was no significance statistically. There’s no statistically significant difference between these two groups, intervention and control in terms of really leading to any changes in their insulin attitude and the degree that any changes in their willingness or lack of willingness to take insulin.
Dr. Bill Polonsky
Instead, everybody improved a bit, but it was in both groups. And when they looked further, they found that it was only less than half who ever bothered to look at more than just one of these pages or this barrier that was identified. In other words, most people looked at nothing or maybe one thing on the website but didn’t really look at it at all.
And they looked further at that is said, let’s look at more engaged people, who really took a look and look at the different things on a website, really drilled down, spent some time there. It turned out that it didn’t really lead to substantially greater benefit at all. So that sounds disappointing, but it leads to these interesting conclusions. And here’s what I think the most important one is from the discussion.
Dr. Bill Polonsky
They said, look, “thus those most likely to benefit may have been least likely to participate and most likely to disengage following enrollment, a phenomenon also observed elsewhere.” That’s the story of our lives, right, Susan? We see this phenomenon every day, and the bottom line is that it leads us to think about the lessons I take away.
Dr. Bill Polonsky
That’s what I want to talk about you guys, is that, you know, look, when you’re dealing with uncomfortable subjects, people I mean, uncomfortable issues, like, “Gosh, I really want to think about taking insulin.” Or “I don’t want to actually aim attention to my blood sugar.” It was probably going to be most useful. It’s actually having a human conversation as opposed to “Go look at this website” when asking people to consider issues that they’d rather not think about.
A human conversation is going to be more likely go better. Scott, you know this even when you live in everyday with type one. We spend a lot of time trying to look at, you know, if we look at the AGP or Dexcom Clarity – it’s fabulous historical data that can help you understand and look at one state over the course of time, but it’s kind of aversive. It’s like saying, why don’t you go balance your checkbook? There aren’t a lot of people who are thrilled about that. But if you and I did it together or there was someone else involved, it’s potentially more possible to take a look at them and make some headway.
And it’s something we see and think about–I think about it all the time. And certainly, one of the things I highlight at the BDI, and Susan and I talked about endlessly, is the people who are most likely to benefit more help most need our help, are more likely to be just miserable in the face of diabetes and disengage are the people least interested in coming to see us!
So it’s this really important challenge. So let me just stop and say, what do you guys think of it?
Scott K. Johnson
I mean, it’s it’s it’s very curious to me. Right. And as someone who is not involved in treatment and clinical discussions like this all the time, and I think like a lot of good research, it leads to many more questions, right? Which deserves some time and attention. And so yeah, it leads to a lot of questions for me.
Dr. Bill Polonsky
That was like a politician’s response.
Dr. Susan Guzman
Haa! He’s good at that. I always think about, you know, as we’re trying to reach more and more people, and one of the requirements that when we get funding is often, you know, how do we scale this? How do we scale this? That’s something that we’re told all the time. And how do we scale human contact, you know, in a way that feels authentic, engaging, respectful, and individualized, and all the things we know really matter to people in general?
Dr. Susan Guzman
And when we’re talking, as Bill said, with very difficult topics like, you know, about considering a medication that I absolutely don’t want to be taking, and yet maybe there are good reasons why I should. But to stand with that discomfort when you’re just supposed to click in on your own, you know that that that website was beautiful and everything. But again, if it’s not something that people will do – whether it’s scalable or not doesn’t matter.
Dr. Bill Polonsky
But I can’t highlight enough how important this publication was and how wonderful that you know Homes-Truscott and colleagues would work so hard to put together such a nice manuscript and to review their data so honestly and say, look, here we have what we know I agree is a really lovely intervention. But the people who you probably most would like to see it will probably never do so.
So I think one of the things they mentioned in the article as well, what about if they were maybe encouraged to look at this when someone’s really being recommended, would that be more likely? Maybe. But my hunch is it really might make a difference if someone was going to sit there. Maybe like a well-trained diabetes educator, a brilliant diabetes psychologist, or even someone who would sit with them and say, let’s you know, I know you’d rather not look at this, but let’s take a look.
Dr. Bill Polonsky
And something about that human teamwork that I don’t know how we’re going to figure out how to scale this on in the way that we’re all told to do so that it’s possible for millions of people to perhaps benefit from, well, new ways of thinking about, for example, insulin. I do have this funny hope that things like AI or ChatGPT might take this, that there might be some way to make this so engaging and interesting that maybe you don’t need human beings involved. Maybe I’m just too old. It’s hard for me to imagine, but I hope it’s possible. I don’t know. What do you guys think?
Scott K. Johnson
I think that there may be something before we get to this point. So the folks in this study were even financially incentivized to look at it. Right? A chance to enter into a drawing for a $100 Amazon gift card or something like that. So there was even some financial incentive, which quite honestly, that does the trick for me a lot of times.
But I think that there’s something prior to this, this engagement and education where a lot of people living with diabetes don’t even want to think about their diabetes or think about thinking about their diabetes. Before we get to what tools we can use to educate them in a positive way and help get rid of some of the stigma and shame. And then beyond that, scaling that good positive education. So it’s like many things with diabetes. You peel off a layer of the onion, and there’s more below to learn and understand.
Dr. Susan Guzman
Diabetes management and diabetes education are very labor intensive. You know, they’re highly hands-on and take a lot of resources. And I’m not sure that what we really want to do that works is available unless there is a way to, you know, maybe integrate AI or something like that, as much as I too hate to say that out loud, I do feel like if we are going to scale some of these interventions, it does have to give people the perception, at least of connection and being individualized and you know, that they can relate to it in a more engaging way.
Dr. Bill Polonsky
And it’s so funny, you know, like we put together interventions like this, and we when we see how little important things can work, you know, like if I provide people videos of their peers, I see someone who’s being successful, how that can make a big difference. All these things can work, but it requires helping people get to the point where they might be willing to actually look at them.
And it’s that aversive quality “take your medicine!” for example, that says, Well, I’d just rather do almost anything else, you know? And that’s why I, I’m humbled in the face of this and in reading this manuscript. It was so well done. It really reminds me of the challenges.
You know, years ago, I should mention, I almost forgotten about this. We put together a conversational workbook on this subject about the different ways you might be worried about going on insulin.
Here are some new ways to think about insulin differently, but it was designed as a conversational workbook that a healthcare provider would talk about with their patient. We were planning and hoping that one of the insulin companies would fund this development. And we had one insulin company that was absolutely thrilled by this. We finally finished our final planning, and they said, “we want to send this out to patients all over the country.” No, no, no. Please don’t send this to anybody. No, the idea is this is a conversational workbook, but it’s designed so you have a conversation.
So we said, “no, we don’t want to do that.” This is a waste of my time and their money. So it remains this interesting odd challenge.
Dr. Susan Guzman
And the other thing I thought of, though, when I read this study was thinking about the project that you did on insulin initiation and the number one thing that predicted someone who was reluctant actually to start, and that was being able actually to experience a saline injection or having someone help you do it right then and there, live and in person and that’s something that you can’t do this where you can watch somebody else do it, you know, virtually.
But that’s not the same thing as going, “before we even talk about it, I want to show you how” because people have all these fears and concerns and previous experiences with injections that are not subcutaneous. Right. So they think, wow, this is going to hurt. And, you know, health care professionals can help them see that a little poke with a very small needle is like, “Oh, wow, that’s it?” That’s an intervention that can’t be done virtually in any capacity, whether there’s a live human on the other end of it or if it’s recorded that requires an experience.
Dr. Bill Polonsky
Yeah, although I might argue the point that actually an online or video approach could be useful, except for what I’m concerned about. I know what you’re concerned about—all the people who will never watch them and have zero interest in looking at them. To me, that’s great. That’s our one big challenge.
I know we shouldn’t just go on forever. We wanted to bring up this issue. We think it’s really important. There’s a strange kind of delight I feel about this, too, which is I guess it gives me a sense of job security that the fact that human conversation, at least for the foreseeable future, is going to be pretty important when we think about how do you support people to be more successful managing your diabetes when almost by definition, it may involve talking about looking at something, They’d rather blow it off and deal with it later.
Scott K. Johnson
I’d go even a step farther than I want to blow it off and look at it later. But I think diabetes is so scary for so many people that they avoid thinking about it at almost all costs, including their diabetes management and, eventually, overall health. I think there are a lot of emotions there that we’re working hard to understand and learn how to help. But there’s a lot left to learn.
Dr. Bill Polonsky
Well, anyway, thanks for all being here. And hats off to Holmes-Truscott and her colleagues for publishing this lovely article that really stimulates our thinking, and I hope it will yours as well. And I turn it over, back to you, Scott.
Scott K. Johnson
Well, just to quickly wrap up, big thanks, as always, to everyone watching. And thank you two for bringing up this important topic and digging into it a bit. It’s always fascinating and enjoyable to learn and talk with both of you. And I’m excited to do it again in our next episode. We’ll see you then.

